Histologic:Chapter 8
Contents
Introduction[edit]
One component of the immune system is lymphatic tissue which consists of reticular connective tissue infiltrated with lymphocytes. This tissue occurs in many regions of the body as diffuse, dense or nodular collections of lymphocytes or as lymphatic organs in which the lymphatic tissue is surrounded by a definite capsule or an epithelium. Lymphatic organs include lymph nodes, thymus, spleen and tonsils.
Lymph Nodes[edit]
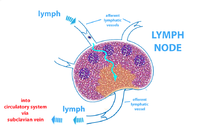
Lymph nodes are round, ovoid or bean-shaped organs found widely distributed in the body. Important groups of lymph nodes occur in chains along the course of blood vessels in such regions as the axilla, groin and mesentery. Lymph nodes are the only lymphatic organs to have an afferent lymphatic supply. They are interposed in the lymphatic drainage of numerous regions of the body. The lymph flowing through the nodes is filtered and phagocytic activity occurs on the particulate matter carried in the lymph. Lymph nodes are important centers for the production of lymphocytes, plasma cells and antibodies. Lymphocytes and antibodies are added to the lymph, which leaves the node by way of the efferent lymph vessels. Lymph nodes are fixed to surrounding connective tissue by loosely arranged fibers that continue into the capsule of the node.
Slide 63: Lymph Node, and Slide 35: Mesenteric Lymph Nodes (H&E)[edit]
Scan these sections with low power to observe the large number of small darkly staining cells. Most of these cells are lymphocytes. On slide 35, study the largest node first.
Identify the capsule of rather dense irregular connective tissue surrounding the lymphatic tissue. Outside the capsule may be seen loose connective tissue containing blood vessels, lymphatic vessels, fat and an occasional nerve.
One of the nodes has an indentation on one side, this is likely the hilus where blood vessels and nerves enter and leave the node, and where the efferent lymphatic vessels exit.
Observe the rounded concentrations of lymphocytes, the lymphatic nodules (primary nodules), in the outer regions (the cortex) of the node. Some of the nodules may have a light central area, the germinal center, indicating that the nodule was active at the time of fixation.
Continue the study of slides 63 and 35 with the medium and high power.
Observe the cortex. The lymphatic nodules and cords of dense lymphatic tissue radiating toward the center of the node are located in the cortex. The cords of dense lymphatic tissue break up into anastomosing medullary cords. The reticular connective tissue framework of the node is obscured by these dense accumulations of lymphocytes.
Look for the medulla in the lymph nodes. This is an inner zone radiating from the hilus. No sharp boundary occurs between the cortex and the medulla, but lymphatic nodules rarely occur in the medulla. Medullary cords of dense lymphatic tissue extend from the lymphatic nodules of the cortex into the medulla. The cords branch and anastomose with each other and are surrounded by the medullary sinuses. The areas between the medullary cords are the medullary sinuses. The sinuses contain reticular cells, reticular fibers, and scattered lymphocytes. The reticular cells are fibroblast-like and electron micrographs show their processes completely enclosing (surrounding) the reticular fibers which they produce.
Identify afferent lymph vessels in the capsule and look for an afferent lymph vessel piercing the capsule to enter the subcapsular sinus. Several of these vessels penetrate the capsule at an angle to bring lymph to the node. These thin-walled, endothelial-lined tubes contain valves and their walls possess very little connective tissue. Afferent lymph vessels are absent at the hilus. Look for efferent lymph vessels in the hilus or near the nodes (slide 35).
Observe the sinuses of a lymph node and attempt to visualize the pathways by which lymph enters, flows through, and leaves a lymph node.
- Identify the subcapsular sinus (marginal sinus) which lies just beneath the capsule and receives lymph from the afferent lymphatics. According to recent reports both macrophages and endothelial cells line the sinuses. Reticular cells can be identified in this comparatively open area.
- The trabecular sinuses, similar in structure to the subcapsular sinus, lie adjacent to the trabecular. These are sometimes called intermediate or cortical sinuses. These areas of diffuse lymphatic tissue allow lymph to flow into the medullary sinuses.
- The anastomosing medullary sinuses occur in the central portion of the lymph node. These are areas of loose lymphatic tissue which lie between the medullary cords and the trabeculae.
- All of the sinuses may contain macrophages that engulf particulate debris and degenerating cells in the lymph. Identify macrophages on slide 63. There are very few on slide 35.
- Efferent lymph vessels collect the lymph from the medullary sinuses.
Slide 63: Lymph Node[edit]
Slide 35: Mesenteric Lymph Nodes (H&E)[edit]
Slide 93: Lymph node (H&E)[edit]
Slide 93, Lymph node (H&E) in the hilus of the lung. These nodes help filter dust, carbon particles, and other debris that get into the lungs.
Note the innumerable macrophages filled with dark, particulate matter. Some of the dark particles may not have been ingested by macrophages or may be deposited after ingestion and rupture of the macrophage.
The node has so many active macrophages that the lymphatic tissue has been greatly reduced. Note the small cortex and only scattered medullary cords, if any.
Lymph Node Details. Since you are now familiar with the general structure of lymph nodes, study the nodes on Slides 35 and 63 in greater detail.
Slide 35: Mesenteric Lymph Nodes (H&E)[edit]
In slide 35 note that most of the lymphatic nodules contain germinal centers containing small and medium-sized lymphocytes, macrophages, and lymphoblasts (few in number).
Small and medium-sized lymphocytes as well as macrophages are more prominent in the germinal centers than are lymphoblasts. The medium-sized lymphocytes have more euchromatin than small lymphocytes, the nucleolus is larger, and the cytoplasm is more basophilic. The macrophages may have an acidophilic, vacuolated cytoplasm and an eccentrically located nucleus.
Slide 63: Lymph Node[edit]
Lymphoblasts (large lymphocytes) are more easily recognized on slide 63, although fewer germinal centers are present on this slide. To identify lymphoblasts, look in the germinal centers for relatively large cells that have basophilic cytoplasm (not very distinct on our slides) and a large mostly euchromatic nucleus with one or two prominent nucleoli.
The germinal centers have a stroma of reticular fibers and reticular cells. Those cells, which have long almost dendritic-like protoplasmic processes, are called dendritic cells. They trap antigens in the presence of antibodies. Dendritic cells are difficult to identify so do not try to find them. Rather, identify the more typical reticular cells in the subcapsular and medullary sinuses on slide 63. Numerous macrophages can also be found in these sinuses.
Observe on your slides that the germinal centers are accentuated by a number of densely packed small lymphocytes that form a ring around the centers. Note that germinal centers are not usually present before birth, nor are they present in animals raised in a germ-free environment.
Thymus[edit]
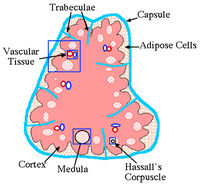
The thymus is unlike other lymphatic organs in two major respects: (1) its stroma consists of a framework of connecting epithelial reticular cells (cytoreticular cells) derived from endoderm. This stroma is not typical reticular connective tissue that is derived from mesoderm and characteristic of other lymphatic organs. (2) Lymphatic nodules are lacking, but the organization of the lobules into a cortex and a medulla may give the unwary student the impression that nodules are present.
Four slides of thymic tissue are to be studied. Slides 55 and 61 are from young individuals. Slide 60 is from a nineteen-year-old, and slide 59 is an involuted thymus from a fifty-year-old person. Since the thymus responds to illness by undergoing stress involution, it should be realized that some sections might not be optimal for studying all features. Slide 55 from a ten-day old child best shows the normal features for a young thymus.
Slide 55: Thymus (Infant) (H&E)[edit]
Observe the thin connective tissue capsule surrounding this organ and the septa (trabeculae) which project inward from the capsule. These strands of connective tissue subdivide the thymus into lobules. Blood vessels are contained within some of the larger septa.
Note that most lobules consist of a darkly stained cortex and a lighter-stained medulla. Reconstructions of the thymus show that the medulla is continuous from one lobule to the next lobule within the same lobe. The palely stained medulla should not be confused with germinal centers of lymphatic nodules. The thymus lacks lymphatic nodules. The medulla stains lighter than the cortex because it contains more epithelial reticular cells and fewer lymphocytes than are contained within the cortex. The epithelial reticular cells are similar in appearance to primitive reticular cells of other lymphatic organs. Identify these in both cortex and medulla.
Identify the acidophilic-staining thymic corpuscles (Hassall’s corpuscles) in the medulla. These structures, unique to the thymus, consist of concentrically arranged epithelial reticular cells. Some of the cells in the center are degenerating. In this young thymus, the thymic corpuscles are small. Note that many are considerably larger on slide 60 and on slide 59.
Note there are no lymphatic sinuses in the thymus but numerous small blood vessels course through the organ. They are located mainly in the septa and the medulla.
In the cortex are some small, rounded clear areas about the size of a large cell. These areas may contain palely stained macrophages, some of which have been active in engulfing other cells.
Study the section under high power. Distinguish between lymphocytes and epithelial reticular cells. Examine the thymic corpuscles closely. Study the macrophages.
Slide 61: Thymus (H&E)[edit]
Slide 61, Thymus, (H&E) is from a seven-year-old child. Identify as many features as possible. Observe how different this thymus appears from the section of the younger thymus previously studied on Slide 55. Slightly more connective tissue and fat are present in the seven-year-old thymus and the thymic corpuscles are larger.
Slide 60: Thymus (H&E)[edit]
Study slide 60, Thymus (H&E) from a nineteen-year-old. Note the reduced number of lobules that are widely separated by a large increase in the amount of fat. Identify the thymic corpuscles. Observe that arterioles, venules, and larger blood vessels are absent from the cortex of the lobules. The thick-walled capillaries that form the blood-thymus barrier are not readily identifiable on our slides.
Slide 59: Thymus (H&E)[edit]
Study slide 59, Thymus (H&E) from a fifty-year-old individual. Compare this involuted thymus with the sections of thymus previously studied.
Tonsils[edit]
Tonsils are defined as aggregates of lymphatic nodules associated with an epithelium. The palatine tonsils, pharyngeal tonsil and lingual tonsils form a ring of lymphatic tissue around the entrance to the throat (pharynx). This protective tonsillar ring is at the oropharyngeal isthmus. The “intestinal tonsils”, better known as aggregated nodules (Peyer’s patches) are located in the ileum of the small intestine.
Palatine Tonsil[edit]
Slide 52: Palatine Tonsil (H&E)[edit]
Observe that “one side,” the surface, is covered by stratified squamous epithelium. From the surface a total of 10 to 20 deeply invaginated epithelial pockets called crypts extend into the substance of the organ. Note that the epithelium lining the crypts is continuous with the surface epithelium. Only a few crypts will be present on any one slide.
On the side of the tonsil opposite the surface epithelium will be found a capsule of dense irregular connective tissue that serves to attach the organ to the wall of the oropharynx. Identify the capsule and the connective tissue septa that extend from it to partially subdivide the organ by separating one crypt from another.
Skeletal muscle and mucous glands occur deep to the capsule.
A large number of lymphatic nodules are present on this section. Many of them have germinal centers. The nodules usually lie as a single layer just beneath the epithelium surrounding each crypt. Only a loose layer of lymphatic tissue separates the nodules from the epithelium. With high power, note that deep in the crypts numerous lymphocytes have infiltrated the epithelium. In some deep areas of the crypts it is difficult to identify the type of epithelium. Observe that the surface epithelium is infiltrated by fewer lymphocytes.
Note that afferent lymphatic vessels and lymph sinuses as seen in lymph nodes are absent from tonsils.
Tonsils are not divided into a cortex and a medulla.
Reticular connective tissue forms the stroma of the tonsil, but the reticular fibers cannot be identified without special stains. The reticular cells are obscured by the lymphocytes.
Aggregated nodules (Peyer’s patches)[edit]
Identify aggregated nodules on slide 31, 168, or 172 Ileum (H&E).
Aggregated nodules (Peyer’s patch) consist of groups of lymphatic nodules massed together in the wall of the ileum opposite the attachment of the mesentery. One Peyer’s patch may consist of ten to seventy lymphatic nodules.
The nodules originate in the lamina propria but they may extend into the submucosa disrupting the muscularis mucosae. Where the nodules project to the luminal surface of the ileum, villi are absent.
Slide 31: Ileum (H&E)[edit]
Slide 168: Ileum (H&E)[edit]
Slide 172: Ileum (H&E)[edit]
Spleen[edit]
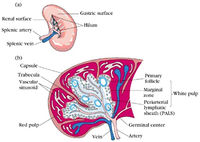
The spleen is an organ which both forms and destroys blood cells. In the embryo the spleen is a fully hemopoietic organ generating all the kinds of blood cells. In late fetal life the spleen stops producing erythrocytes and granulocytes, but it continues to generate lymphocytes and monocytes. However, it retains full hemopoietic potentialities so that pathologically, in adulthood, the spleen may once again initiate the functions of red bone marrow. The spleen is highly active in the production of antibodies. Plasma cells are the main source of the antibodies. The spleen also serves as a specialized blood-filtering organ and it can serve for the temporary storage of platelets and erythrocytes.
Slide 18: Spleen (H&E)[edit]
Examine slide 18, Spleen (H&E) and identify the capsule and trabeculae
The capsule is covered by mesothelium. The capsule is composed of collagen, elastic and a very few smooth muscle fibers. The elastic fibers predominate in the inner half of the capsule.
Note that the trabeculae appear to be cut at random and that they stain similar to the capsule since they are extensions of this structure into the substance of the spleen. Trabeculae form a supporting framework.
The amount of elastic tissue in the trabeculae is similar to that found in the inner half of the capsule. Note that some sections of the trabeculae show trabecular arteries and veins coursing through them. Neither demonstrates an adventitia; the connective tissue of the trabecula immediately surrounds the media.
Identify the darkly stained lymphatic nodules (splenic nodules) of the white pulp. Identify the central arteries passing through a lymphatic nodule. Note that diffuse to dense lymphatic tissue also occurs in the white pulp mainly surrounding and following the distribution of the arterial vessels. White pulp is typical lymphatic tissue containing a stroma of reticular cells and fibers.
Select a particularly dense or large lymphatic nodule to identify the marginal zone at its periphery. The marginal zone is a transitional region of red pulp containing more lymphocytes and plasma cells than the pulp cords. Branches from the central artery pass into this transitional zone. It is here that T- lymphocytes leave the general circulation to take up residence in the spleen.
The red pulp occurs mainly as venous sinuses and the intervening pulp cords. This tissue lies between the areas of the white pulp. There is no sharp boundary between red and white pulp. The red pulp is atypical lymphatic tissue. It has reticular connective tissue infiltrated with lymphocytes and monocytes, but in addition, all other kinds of blood cells occur here as well. Especially numerous are the erythrocytes which impart a reddish coloration to the area of the red pulp in the fresh spleen.
Slide 19: Spleen (PASH)[edit]
The pulp cords consist of the tissue occupying the narrow areas between the venous sinuses. With high power, study the splenic sinuses and pulp cords. Note how much easier it is to identify the venous sinuses by using the PASH stained section of Spleen (slide 19, Spleen PASH).
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Nodular hyperplasia of the prostate--characterized by large discrete prostatic nodules--is a common disorder in men over 50 years of age. The nodules cause the prostate to be enlarged and to have an increased weight. The human prostate is surrounded by a restrictive capsule. These nodules cause increased pressure within the capsule which leads to constriction of the urethra as it passes through the prostate. Urethral constriction leads to retention of urine.