Histologic:Chapter 6
Contents
Introduction
Nervous tissue is highly specialized to form the nervous system which is organized into two major divisions: The central nervous system and the peripheral nervous system. The central nervous system consists of the brain and spinal cord. The peripheral nervous system consists of all the nervous tissue lying outside of the brain and the spinal cord. This is subdivided into the cerebrospinal portion (the 12 pairs of cranial nerves, 31 pairs of spinal nerves and associated ganglia) and the autonomic nervous system (sympathetic and parasympathetic components) which deals with visceral activities (smooth muscle, cardiac muscle, and glandular secretions). These parts of the nervous system are not separate entities but are structurally and functionally interdependent. The nerves of the peripheral nervous system are widely distributed throughout the body, extending into all tissues and organs.
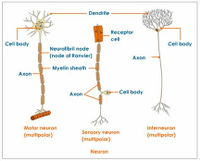
The structural and functional unit of the nervous system is the neuron, which is defined as a nerve cell body and all of its processes. Nerve cell bodies are located with the CNS and in the various ganglia outside of the CNS. The processes are dendrites and axons. Neurons function in cooperating groups or chains, some receiving the excitation and passing it on to others, often in many relays, until somewhere in the body a response is affected. Structurally, neurons are classified as multipolar, bipolar, and unipolar according to the number of processes arising from the cell body.
A nerve is a collection or aggregation of nerve fibers outside the CNS, surrounded by a sheath of connective tissue and supported by connective tissue stroma. A nerve fiber consists of an axonal process enveloped with one or two sheaths (myelin sheath and/or neurolemma or Schwann’s sheath).
A ganglion is a group of nerve cell bodies located outside of the central nervous system. These are termed: cranial ganglia, dorsal root ganglia, sympathetic ganglia, and parasympathetic ganglia.
Nerve Fibers And Nerves
Slide 27: Peripheral Nerve (Osmium), Cross and Longitudinal Sections
Osmium stains myelin, therefore the myelin sheaths will be black, unmyelinated fibers are vaguely outlined, other structures do not stain.
These are sections of a typical peripheral nerve, which contains myelinated fibers of various sizes as well as unmyelinated fibers. Note--axons always shrink in routinely prepared sections.
Look first at the cross section.
Note the epineurium surrounding the entire nerve and sending extensions between the fasciculi (interfascicular CONNECTIVE TISSUE).
Note perineurium surrounding each large fasciculus of nerve fibers. The “cracks” or spaces in some of the fasciculi were sites of smaller perineurial septa.
Within each fasciculus, note myelinated nerve fibers of different sizes. The axon may be faintly apparent (shrunken) or completely unstained.
Focus carefully to see very small thinly myelinated fibers. Unmyelinated fibers are virtually impossible to distinguish.
Look at the longitudinal section
Identify the same structures as above, also fat cells stained with osmium, in the epineurium.
In good longitudinal sections of the larger fibers look for the nodes of Ranvier, but they are not easily seen because of tissue contraction.
Slide 50: Peripheral Nerve (Masson’s Stain)
Connective tissue stains blue, nuclei are dark blue, and myelin is orange-red.
Repeat the study of the cross and longitudinal sections as for slide 27 but now detailed structure can be seen. The perineurium should stain blue, but it may be partially red, probably because of inability of the blue stain to completely penetrate this dense tissue.
Note especially that perineurial septa and endoneurium are seen distinctly. The nuclei that appear to be in the endoneurium are fibroblast nuclei of the endoneurium and neurolemma cell (Schwann cell) nuclei; do not try to distinguish between them, but the majority are neurolemma (Schwann) nuclei.
In the nerve fibers, the axon may or may not be stained. Myelin is partly removed from the myelin sheath, leaving the neurokeratin network.
Slide 13: Peripheral Nerve (H&E)
Check the same features as previously described, in this cross-section, to see their appearance with a routine stain.
Central Nervous System: Brain
The central nervous system (CNS) comprises the brain and spinal cord. These areas contain nerve cells and their processes, along with specialized support cells.
The specialized support cells of the CNS are collectively called glia. These are astrocytes, oligodendrocytes, ependyma and microglial cells. Astrocytes are stellate cells that are involved in fluid transport and structural support. The stellate morphology is not evident in conventional H&E sections because the processes merge with the processes of other cells, but is seen with special staining methods. Two types of astrocyte have been identified. Fibrous astrocytes are most evident in the white matter and have long cell processes which are rich in bundles of glial fibrillary acidic protein (GFAP). Protoplasmic astrocytes are most evident in the gray matter of the brain and have long thin processes containing few bundles of GFAP.
One important structural adaptation of astrocytes is seen in their interaction with the blood vessels of the brain, which they surround by forming flat plates termed end feet. The interaction induces changes in the structure of the cerebral vascular endothelium, rendering it highly impermeable, so that it acts as a barrier to diffusion between the blood and the brain, the “blood-brain-barrier”.
Oligodendrocytes are the myelin-producing cells of the CNS, each cell sending out several cell processes and myelinating several nearby axons. In routine histologic sections their branching morphology is not seen, but they do show a rounded nucleus with moderately dense-staining chromatin and, in most preparations, a cytoplasm containing a clear ‘halo’ around the nucleus. Such a halo is an artifact of preparation because oligodendrocytes are fragile and contain few cytoskeletal elements.
Ependymal cells are epithelial like cells that line the cavities in the brain (ventricles) and the central canal of the spinal cord, forming a sheet of cuboidal cells in contact with the cerebrospinal fluid. Each ependymal cell has a small oval basal nucleus with dense chromatin, and many are ciliated. Unlike other epithelial cells, the ependymal cells do not lie on a basement membrane but have tapering processes which merge with the processes of underlying astrocytic cells.
The CNS has its own unique set of immune cells, the main type being the microglial cells, which are specialized macrophages. In conventional H&E preparations microglial cells are not easily seen, appearing only as rod-shaped nuclei with no discernible cytoplasmic borders. The phenotype of microglia suggests that they are similar to dendritic antigen-presenting cells, having a low level of phagocytic activity and expressing class II major histocompatibility molecules.
In disease states microglial cells become activated and increase in size and number. Under these circumstances they are usually supplemented by monocytes, which enter the brain from the blood and form macrophagic cells. The brain appears to have only a very small traffic of lymphoid cells in the normal state.
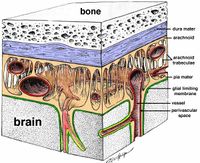
The CNS has three protective coats, the meninges, which are composed of fibrocollagenous support tissue and epithelial cells. These three layers are: the dura, the arachnoid and the pia.
The dura is a tough fibrocollagenous layer, which forms the outer coat of the CNS. It blends with the periosteum of the skull and is attached to the periosteum of the vertebral canal by the dentate ligaments. It is covered on its internal surface by an incomplete layer of flat epithelial cells. The dura is reflected down from the skull to form sheets of tissue, the tentorium cerebelli and the falx cerebri, which separate the structures of the brain. The venous sinuses of the brain run at the base of these sheets of dura. The arachnoid is a layer of fibrocollagenous tissue covered by inconspicuous flat epithelial cells and is located beneath, but not anchored to, the dura. Web-like strands of fibrocollagenous tissue extend down from the arachnoid into the subarachnoid space, which contains the cerebrospinal fluid. The main arteries and veins to and from the brain run in the subarachnoid space.
The pia is a delicate layer of epithelial cells associated with loose fibrocollagenous tissue. It lies external to a basement membrane which completely surrounds the CNS.
Slide 72: Cerebral Cortex (H&E)
With H&E, the meninges as well as the various layers of the cerebral cortex are visible. Distinguish the general regions of the cerebral cortex:
- White matter.
- Note few cells per unit area. Cells in the white matter are microglia with few if any neuron bodies.
- Gray matter (cerebral cortex).
- The cerebral cortex is divided into six layers. Distinguishing the exact borders of these layers is difficult requiring special staining and is beyond the scope of this discussion. The six layers from outside to inside include: plexiform or molecular layer, small pyramidal cell layer, medium pyramidal cell layer, granular layer, large pyramidal cell layer, and the polymorphic cell layer.
- Meninges consisting of the pia mater.
Slide 14: Cerebellum (H&E)
The outer portion of the cerebellum, the cortex, is made up of a molecular layer and a granular layer. At the junction between these two layers are the large cell bodies of Purkinje cells. These cells are characteristic of cerebellum. They contain numerous dendrites that extend into the molecular layer and a single axon.
The central portion of the cerebellum consists of myelinated fibers which make up the white matter.
The choroid plexuses are located in the ventricular system of the brain and produce cerebrospinal fluid. Each choroid plexus consists of a vascular stroma covered by columnar epithelial cells, which form large frond-like masses. The cerebrospinal fluid produced in the ventricles flows out through exit foramina at the base of the brain and circulates in the subarachnoid space. It is reabsorbed by the venous sinuses in the dura.
Slide 15: Choroid plexus (Masson)
On this trichrome stained section of choroid plexus note the multiple fronds of tissue. Each is covered with ependymal cells and has a connective tissue infrastructure.
Spinal Cord: General Structure
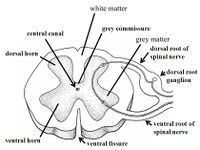
The spinal cord is composed of two principal parts extending the length of the cord, the inner core of gray matter and an outer layer of white matter. The entire cord is supported in a framework of neuroglia. In the most peripheral part of the cord, processes of fibrous astrocytes condense to form the marginal glial membrane, in which nerve fibers are absent.
The gray matter is in the form of two large lateral masses connected by a narrow strip across the midline, the gray commissure, in which lies the central canal, which is largely obliterated in the adult. Each lateral gray mass has a dorsal gray horn or column, a ventral gray horn or column, and an intermediate gray area. The configuration of the gray matter varies in different parts of the cord; the ventral horns are widest in the cervical and lumbar enlargements in which are located the anterior horn cells that innervate the upper and lower extremities respectively, and narrowest in the thoracic segments.
All neuron cell bodies, together with their dendrites and initial portions of their dendrites and initial portions of their axons, are in the gray matter. Unmyelinated nerve fibers course everywhere as well as some myelinated fibers (terminations of incoming sensory fibers or tract fibers in the white matter). Blood vessels are prevalent.
The white matter is composed of nerve fibers, most of which are myelinated, connective tissue septa with blood vessels coming in from the pia matter, and neuroglia septa. Dorsal roots (incoming sensory fibers) are attached to the dorsal lateral surface of the cord (dorsolateral sulcus), and ventral roots to the ventrolateral surface (ventrolateral sulcus). In relation to these, the white matter is divided into the dorsal white columns, lateral white columns, and ventral white columns. Ventrally, there is a deep medial ventral fissure, and dorsally a shallow medial sulcus. The cord is covered with meninges consisting of the outermost thick fibrous dura mater, a subdural space, the arachnoid and subarachnoid space with arachnoid trabeculae which contains cerebrospinal fluid, and the pia mater, a fibrous membrane attached to the spinal cord. The latter two membranes are often referred to as the pia-arachnoid. From the pia mater, connective tissue septa carrying blood vessels penetrate the white and gray matter.
When dorsal root fibers enter the cord and ventral root fibers first leave the cord, they lie in the subarachnoid space. As they move laterally to exit through the intervertebral foramina, the dura mater continues over them as epineurium. The arachnoid fades out quickly.
Slide 97: Lumbar Cord With Meninges, Three-Year Old Child (H&E)
With H&E, details of neuron cell bodies are seen quite well; other tissues stain much as in other organs.
Distinguish the general regions of the cord:
- The H-shaped gray matter with its dorsal gray columns, the broad ventral columns, and the intermediate gray area.
- The white matter with its three divisions.
- The delicate dorsal medial (posterior) septum of neuroglia and the ventral fissure.
- The thick dura mater (dense fibrous connective tissue) - the outermost layer of the meninges.
- The central canal in the gray commissure. It is lined with ependymal cells, which have a columnar shape; some may have flagella.
White matter.
- Note innumerable myelinated fibers, mostly in cross sections, since these are mainly ascending and descending tracts. Myelin is not preserved; a clear space remains. The axon is unstained or faintly seen, or it may not be present.
- Thin connective tissue septa and small blood vessels can be seen. Look for perivascular spaces around the blood vessels - clear spaces that are actinically enlarged due to shrinkage of tissues.
- The numerous small nuclei seen are mainly those of fibrous astrocytes and oligodendroglia.
- Identify the marginal glial membrane. It forms the most peripheral part of the spinal cord, is formed by processes of fibrous astrocytes, and lacks nerve fibers.
Dorsal gray columns.
- Note the uppermost large pale area (substantia gelatinosa), the more fibrillar base of the dorsal horn, and myelinated fibers sweeping into these areas from the dorsal white columns (incoming sensory fibers).
- The small nuclei are astrocyte and oligodendroglia nuclei. Small neuron cell bodies are not easily seen.
- Some of the sections may show the actual entrance of the dorsal roots.
Ventral gray columns - general. The columns are broad.
Note the meshwork of fine fibers throughout (unmyelinated nerve fibers, processes of astrocytes), nuclei of astrocytes and oligodendrocytes, small blood vessels in their perivascular spaces, and large anterior horn cells.
The anterior horn cells (Motor Neurons)
- In sections, entire cells are rarely seen, but note the multipolar shapes of the cells, parts of cell processes, Nissl bodies, in the neuroplasm and the distinctive nucleus and nucleolus. Dendrites are short processes that contain Nissl bodies. Look for a cell that shows a clear axon hillock and an emerging axon.
- Note the perineuronal space (exaggerated in sections) around each cell body with occasional perineuronal satellite cells close to the cell body. Satellite cells are astrocytes and/or oligodendrocytes.
- Axons of these anterior horn cells can be seen in groups passing down into the ventral white matter to emerge to form the ventral roots. They innervate the muscles of the lower extremities.
- Innumerable nuclei of neuroglia cells are seen everywhere throughout the gray matter; their cytoplasmic processes shrink to invisibility. Identify astrocytes and oligodendrocytes.
Astrocytes have rounded, somewhat lightly-staining (vesicular) nuclei; they vary in size.
Oligodendrocytes have small, darker-stained nuclei, much like a miniature lymphocyte.
Microglia are not as numerous nor as easily identified (do NOT try to identify them). Microglia are phagocytic cells derived from monocytes.
Look for very small internuncial (connector) neurons scattered throughout the ventral gray. They are typical, but small, neurons. These are interposed between sensory and motor neurons in reflex pathways.
Meninges of the spinal cord.
- Distinguish the pia mater of fibrous connective tissue immediately around the cord.
- In the subarachnoid space, note bundles (fasciculi) of nerve fibers - rootlets of dorsal and ventral roots.
- Distinguish the arachnoid membrane (if not torn) forming the peripheral boundary of the space - a thin connective tissue membrane covered with a layer of squamous cells. It sends fine trabeculae across the space.
- The dense fibrous dura mater lies external to the arachnoid. A subdural space lies between the dura and arachnoid.
Sympathetic Chain Ganglion With Multipolar Neurons
These are the post-ganglionic visceral efferent neurons. Axons of neurons in the lateral sympathetic nucleus of the thoracic cord had come to the sympathetic chain via the white rami communicantes. Many have synapsed on these ganglion cells. (Others pass through the chain to synapse elsewhere.)
Slide 16: Sympathetic Ganglion (H&E)
This ganglion has an epineurium but many ganglia do not show such a distinct capsule.
The ganglion cells are more loosely arranged than in the spinal ganglion. Connective tissue stroma is more apparent, also septa with blood vessels.
Ganglion cells are more uniform in size. All are multipolar.
Note typical characteristics of neuron cell bodies: nuclei may be eccentrically placed, an occasional cell is binucleated, and a few cells have yellow pigment. These are normal features of sympathetic ganglion cells.
Perineuronal spaces are less constant, satellite and capsule cells are more variable in number but are present.
Nerve fibers in the stroma are largely unmyelinated or finely myelinated, and less easily identified with routine stains.
Parasympathetic Ganglia
These are in the walls of organs. Preganglionic parasympathetic fibers go from the cell bodies in the brain stem or sacral spinal cord to the organs to be innervated and synapse on small, typical multipolar neuron cell bodies in ganglia (post-ganglionic neurons). Postganglionic fibers (axons) of these are then distributed to smooth muscle and glands.
Slide 94: Colon (H&E)
Between the two muscle layers of the esophagus and all subsequent parts of the digestive tract, is a chain of parasympathetic ganglia and vagus nerve fibers (myenteric plexus of Auerbach). The fibers are finely myelinated or unmyelinated. Groups of ganglion cells are seen intermittently within the chain. Look for lightly stained areas between the muscle layers and note:
Small nerves surrounded by a thin perineurium. The numerous nuclei within the nerve are nuclei of neurolemma cells (Schwann cells) or fibroblasts of the endoneurium.
Varying numbers of multipolar ganglion cells (only parts of cells may be seen).
Look for a complete cell that shows the characteristic nucleus and nucleolus. Nuclei may be eccentrically located.
Perineuronal spaces, capsule cells, and satellite cells are present but not as consistent as in the large dorsal root ganglion cells.
The interstitial material is unmyelinated nerve fibers and endoneurium.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||