Histologic:Chapter 10
Contents
- 1 Olfactory Area
- 2 Epiglottis
- 3 Trachea
- 4 Bronchi, Bronchioles, and Lung
- 4.1 Slide 93, Hilus (Root) of the lung, adult male. (H&E)
- 4.2 Slide 33, Lung, bronchi, bronchioles, human child (H&E)
- 4.3 Slide 105, Lung (H&E)
- 4.4 Slide 108. Lung with Pleura (Masson’s stain)
- 4.5 Slide 106, Lung with Pleura (Verhoeff’s stain)
- 4.6 Slide 112. Lobar (secondary) Bronchi, 28 year-old male (H&E)
- 4.7 Slide 110. Segmental bronchus (branch of a lobar bronchus), 62 year-old male (H&E)
Olfactory Area
Slide 101, Olfactory Area (H&E, thick celloidin section)
Slide 101 is a straight piece of tissue, representing only a small portion of olfactory area.
With low power, identify the general regions:
- Olfactory mucosa - epithelium and lamina propria with glands and nerves.
- Bone (ethmoid bone) on which the mucosa rests (it may be mechanically separated from the bone in places).
- Connective tissue and fat below the bone.
Olfactory epithelium
- Recognize it as a pseudostratified columnar type.
- Note the tall sustentacular cells with ovoid nuclei that are in the upper portion of the epithelium. Details cannot be made out in this thick section.
- The more rounded nuclei in the deeper layers are nuclei of bipolar neurons, the olfactory cells. The cilia on the free surface of the epithelium are on the distal processes of olfactory cells; the thickness of the section makes them appear as a continuous border which is not so; they are actually in tufts. The light zone below the nuclear layers is cytoplasm of the cell body of olfactory cells; cell outlines are not distinct.
- Note rounded nuclei of small basal cells.
The lamina propria consists of loose connective tissue.
- Note the branched tubuloalveolar olfactory glands of Bowman. Cells are large, more or less cuboidal or low columnar, have very granular cytoplasm (indicates secretory) and rounded nuclei. Look for sections of ducts passing toward the epithelium and through it.
- Note sections of nerves (unmyelinated fibers) - the fila olfactoria - made up of axons of the olfactory cells.
- The lamina propria merges with the periosteum of the underlying bone.
Bone - seen in longitudinal section.
- Identify lamellae of bone and osteocytes in lacunae. The bone on the straight sections is younger than that in the scroll sections, and may show osteoblasts and some osteoclasts.
Epiglottis
Slide 111, Epiglottis, (H&E)
This is a section through the body and tip of the epiglottis from a 28 year-old man. The oral (anterior) surface is at the top of the section, the laryngeal (posterior) surface at the bottom.
The epithelium. The upper surface is stratified squamous epithelium. Follow it over the tip of epiglottis. It continues for some distance but the connective tissue papillae disappear. It changes gradually to an intermediate type, and eventually to pseudostratified ciliated columnar epithelium with goblet cells. Surface cells of this latter type may be torn. Look for occasional taste buds in the posterior epithelium.
Lamina propria -- the layer of fine-fibered loose connective tissue of varying thickness with diffuse lymphatic tissue. An occasional lymphatic nodule may be present.
Submucosa - the deeper loose connective tissue layer is interspersed with adipose tissue and groups of tubuloalveolar mixed glands that vary in number in different sections. Look for small ducts among the alveoli, and larger ones coursing toward the surface of the section. Note small blood vessels, lymphatics and nerves in both the lamina propria and the submucosa.
Elastic cartilage - forms the central plate of the epiglottis. It is a single cartilage of variable thickness but in sections may appear as separated pieces.
Trachea
Slide 109, Trachea, 62 year old man (cross-section, H&E)
The trachea has a series of C-shaped cartilage plates for support. In this section the entire “C” cannot be seen. The tissues that make up the wall of the trachea are arranged in orderly sequence that set the pattern for the bronchi. However, the smooth muscle is confined to the region between the ends of the C-shaped cartilage plates.
On slide 109 is half of a cross-section of a complete trachea. The trachealis muscle is at the left end of the section in the microscopic field. There are mechanical separations in the tissues in some regions.
Select an area for study where the layers of the wall can be seen in good sequence. Look for blood vessels and nerves in all regions.
Mucosa
- Identify the typical pseudostratified ciliated columnar epithelium with goblet cells, and the thick basement membrane. In some areas, the epithelium seems to have undergone metaplasia and changed to a low stratified squamous type or an intermediate type.
- Note the lamina propria of fine-fibered loose connective tissue with scanty diffuse lymphatic tissue and a thick elastic membrane in its deeper part; elastic fibers are in cross-section, since the membrane courses longitudinally.
Submucosa with tubuloalveolar mixed glands. The alveoli show postmortem changes; cells are not always clearly defined and nuclei are dark and shrunken. Look for ducts within the glands and coursing toward the surface. Some adipose tissue is present; it is not a usual constituent of the submucosa.
Cartilage layer with perichondrium. Note how the perichondrium blends with the connective tissue of the submucosa and the fibrosa. Dark blue granular material seen in cartilage is calcium deposits -- a frequent occurrence in older individuals.
Fibrosa -- the connective tissue external to the perichondrium and blending with looser connective tissue that connects it with adjacent structures. Adipose tissue is present.
Trachealis muscle -- fibers course mainly transversely. It is in the submucosa, may be intermingled with the glands, and may extend into the fibrosa.
Slide 2, Trachea, Adult (cross section, H&E)
Since mature cartilage is difficult to section, it tends to tear, and softer tissues around it may tear or even break away.
Look at the section grossly. Note that it is flattened on one side. This is the “open end” between the ends of the C-shaped cartilage. The cartilage may not be present as a complete C; it may appear in pieces, due to not being of equal thickness throughout its extent.
Study a section through the wall and identify all layers and tissues as in slide 109. Find an area where the epithelium is intact; it is partially or completely stripped off in places. Note prominent secretory granules in many of the serous cells of the mixed glands.
Study the trachealis muscle region. The muscle fibers insert into the inner surface of the ends of the cartilage by small elastic tendons (not seen).
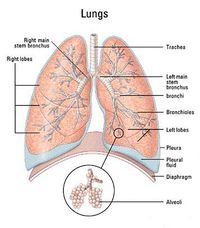
Bronchi, Bronchioles, and Lung
Slide 93, Hilus (Root) of the lung, adult male. (H&E)
Embedded in the connective tissue of the hilus (root) of the lungs are all the structures that enter or leave the lungs. This slide has a section of the pulmonary artery, a hilar lymph node, and a part of the primary bronchus. The large pulmonary veins are not present.
Pulmonary artery
- Find and identify its large artery structure: layers of elastic lamellae interspersed with smooth muscle fibers. Nuclei of the latter are prominent, cell outlines are indistinct (fibers course obliquely).
Hilar lymph node. Dust cells from the lung tissue deposit their dust and carbon particles in these nodes.
- Macrophages loaded with carbon deposits are so numerous that the internal structure of the node is obscured.
- At the periphery of the node are seen the subcapsular sinus and parts of cortical nodules.
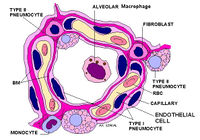
Lung Tissue.
- Look for small pulmonary artery branches; they are accompanying bronchioles but are difficult to see.
- Pulmonary venules may be seen in thin connective tissue septa.
- Identify pulmonary alveoli; many are in cross sections, some may show the cup-shape with an open end; they are lined mainly with a simple squamous epithelium. Congested capillaries give prominence to the interalveolar septa, but obscure detailed structure of alveoli.
- The large open spaces are alveolar ducts. In a good longitudinal section, pulmonary alveoli making up their wall may be seen.
Slides 106, and 108 are from animals, and slide 33 is from a child. Each slide does not contain all the desired structures but between them, a total picture can be conceived. Slides 110 and 112 are from an adult male. The bronchi are much larger, and are typical for bronchi of those sizes.
Slide 33, Lung, bronchi, bronchioles, human child (H&E)
Much of the lung tissue is too pathological for study but the conducting tubules are intact.
Identify the lobar (secondary) bronchus and its artery and check the structure of its wall. An accompanying pulmonary vein is present on the opposite side of the bronchus from the artery. These larger branches of the pulmonary veins have elastic fibers interspersed with the muscle, but not elastic lamellae as in the arteries.
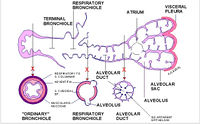
Bronchioles. There are 4 or 5 divisions of bronchioles. Cartilage and glands are absent, but epithelium, lamina propria, muscularis and fibrosa are still present. The first divisions from the subsegmental bronchi have good pseudostratified ciliated columnar epithelium. In subsequent divisions, this epithelium decreases in height, goblet cells disappear. The final divisions, the terminal bronchioles, have simple columnar ciliated epithelium. The muscularis becomes relatively more prominent as the tubules decrease in size.
Respiratory bronchioles. These are smaller tubules with a rigid lumen, low columnar or cuboidal epithelium, prominent myoelastic layer (muscle is seen distinctly). The epithelium may be sloughed off during sectioning but the myoelastic layer identifies the tube as a respiratory bronchiole. Pulmonary alveoli may pouch off the wall on the side opposite the pulmonary artery. Look for respiratory bronchioles in cross sections, and for ones that are giving rise to alveolar ducts.
In the area of normal lung tissue, again study structure of alveolar ducts and alveoli. Capillaries here are greatly congested.
Slide 105, Lung (H&E)
Look for bronchioles and respiratory bronchioles and their accompanying arteries. Branches of pulmonary arteries are atypical in that elastic lamellae are continued into even the smallest branches where only two or three layers are present.
Again, study alveoli and alveolar ducts and sacs. The “knob’s” of smooth muscle at the openings of the alveoli are seen better here than in previous slides.
Slide 108. Lung with Pleura (Masson’s stain)
Look at lung tissue and whatever other structures are present as they appear with this stain.
Slide 106, Lung with Pleura (Verhoeff’s stain)
Note the distribution of elastic fibers in the lung tissue, in blood vessels and other structures.
Look especially for fine elastic fibers in the interalveolar septa.
Slide 112. Lobar (secondary) Bronchi, 28 year-old male (H&E)
The section was taken just as a primary bronchus has divided to form two lobar bronchi. This slide has a good single bronchus.
Components of the wall continue to be like those in the trachea and large bronchi but smooth muscle has spread out to encircle the lumen, so that there is a complete layer of muscle all around the bronchus.
Study the single bronchus. Disregard the debris in the lumen. Note that the cartilage plates are large and close together. Epithelium is intact in places but may be partly sloughed or covered with debris elsewhere.
Select an area where layers in the wall of the bronchus are seen in orderly fashion, and identify the layers and structures within each layer.
- Mucosa: epithelium, lamina propria with lymphocytes, thin elastic membrane, and muscularis.
- Submucosa with glands
- Cartilaginous layer
- Fibrosa
- Look for small bronchial vessels, nerves and possibly small parasympathetic ganglia in the wall of the bronchus.
Identify the pulmonary artery, a small branch of the pulmonary vein (not on all slides), small nerves, and the hilar lymph nodes.
Slide 110. Segmental bronchus (branch of a lobar bronchus), 62 year-old male (H&E)
Study the bronchus as in slide 112. The structure is similar except that the cartilage plates are smaller and farther apart.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||