Difference between revisions of "Histologic:Chapter 12"
(→Gallbladder) |
(→Gallbladder) |
||
| (4 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
== Introduction == | == Introduction == | ||
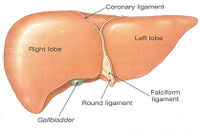
| − | + | [[File:HistologicChapter12Liver.jpg|thumb|200px|Liver Lobe]] | |
The liver functions as a vast biosynthetic chemical factory, synthesizing large complex molecules from substances brought to it in the blood, particularly substances recently absorbed by the intestine and transported by the portal blood system. All of the biochemical functions of the liver are carried out by the epithelial parenchymal cells of the liver, the hepatocytes. Hepatocytes are responsible for bile synthesis and secretion, excretion of bilirubin, protein carbohydrate and lipid metabolism, storage (vitamins A, D and B12 and iron as ferritin), and conjugation and elimination of metabolites and toxins. | The liver functions as a vast biosynthetic chemical factory, synthesizing large complex molecules from substances brought to it in the blood, particularly substances recently absorbed by the intestine and transported by the portal blood system. All of the biochemical functions of the liver are carried out by the epithelial parenchymal cells of the liver, the hepatocytes. Hepatocytes are responsible for bile synthesis and secretion, excretion of bilirubin, protein carbohydrate and lipid metabolism, storage (vitamins A, D and B12 and iron as ferritin), and conjugation and elimination of metabolites and toxins. | ||
| Line 8: | Line 8: | ||
=== Blood Supply to a Lobule === | === Blood Supply to a Lobule === | ||
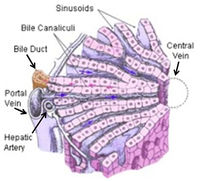
| − | + | [[File:HistologicChapter12Liver2.jpg|thumb|200px|Liver]] | |
At the periphery of the lobules, in the angles between 2 or 3 adjacent lobules, lie the interlobular septa or portal canals consisting of connective tissue, and containing a branch of the hepatic artery, a branch of the portal vein, a small bile duct, a lymphatic vessel and small nerves. The blood that enters a lobule is supplied from the vessels in the portal system. Both venous and arterial blood enters a lobule. The venous blood enters the sinusoids directly from the smallest branches of the portal vein. Only a small volume of arterial blood enters the sinusoids directly from the smallest branches of the hepatic artery. Most of the arterial blood goes through a capillary bed to enter the small branches of the portal vein before going on to the sinusoids. Blood in the sinusoids “bathes” the hepatocytes before passing into the central vein from which it flows into a sublobular (intercalated) vein. Sublobular veins progressively unite to form the collecting veins that progressively join to form the hepatic veins. Two or more hepatic veins empty directly into the inferior vena cava. | At the periphery of the lobules, in the angles between 2 or 3 adjacent lobules, lie the interlobular septa or portal canals consisting of connective tissue, and containing a branch of the hepatic artery, a branch of the portal vein, a small bile duct, a lymphatic vessel and small nerves. The blood that enters a lobule is supplied from the vessels in the portal system. Both venous and arterial blood enters a lobule. The venous blood enters the sinusoids directly from the smallest branches of the portal vein. Only a small volume of arterial blood enters the sinusoids directly from the smallest branches of the hepatic artery. Most of the arterial blood goes through a capillary bed to enter the small branches of the portal vein before going on to the sinusoids. Blood in the sinusoids “bathes” the hepatocytes before passing into the central vein from which it flows into a sublobular (intercalated) vein. Sublobular veins progressively unite to form the collecting veins that progressively join to form the hepatic veins. Two or more hepatic veins empty directly into the inferior vena cava. | ||
| Line 73: | Line 73: | ||
Remember that lymph and bile flow from a lobule in a direction opposite to the flow of blood in the sinusoids. | Remember that lymph and bile flow from a lobule in a direction opposite to the flow of blood in the sinusoids. | ||
| − | ==== Slide 152, Liver and Gallbladder ==== | + | ==== Slide 152, Liver and Gallbladder (H&E) ==== |
<peir-vm>UAB-Histology-00152</peir-vm> | <peir-vm>UAB-Histology-00152</peir-vm> | ||
| Line 80: | Line 80: | ||
== Gallbladder == | == Gallbladder == | ||
| − | + | [[File:HistologicChapter12GallbladderDiagram.jpg|thumb|200px|Gallbladder Diagram]] | |
The pear-shaped gallbladder shows marked variation in size and shape among different individuals. Anatomically, it consists of a neck, a body, and a blindly ending fundus. Histologically, its wall consists of a mucosa, a muscularis, a perimuscular layer of connective tissue, and a serosa or fibrosa. | The pear-shaped gallbladder shows marked variation in size and shape among different individuals. Anatomically, it consists of a neck, a body, and a blindly ending fundus. Histologically, its wall consists of a mucosa, a muscularis, a perimuscular layer of connective tissue, and a serosa or fibrosa. | ||
| − | === Slide 151 | + | === Slide 151 Gallbladder, (H&E) === |
Mucosa - The mucosa consists of an epithelium, its basement membrane, and an underlying lamina propria of loose connective tissue. The tall, simple columnar epithelial cells of the mucosa are absorptive in nature. They have basal ovoid nuclei and on their luminal surface is a thin striated border (demonstrated by EM). No goblet cells are present in this epithelium. The mucosa of the non-distended gallbladder is irregularly folded, somewhat resembling villi when it is sectioned. These folds largely disappear when the gallbladder is filled. | Mucosa - The mucosa consists of an epithelium, its basement membrane, and an underlying lamina propria of loose connective tissue. The tall, simple columnar epithelial cells of the mucosa are absorptive in nature. They have basal ovoid nuclei and on their luminal surface is a thin striated border (demonstrated by EM). No goblet cells are present in this epithelium. The mucosa of the non-distended gallbladder is irregularly folded, somewhat resembling villi when it is sectioned. These folds largely disappear when the gallbladder is filled. | ||
| Line 97: | Line 97: | ||
<peir-vm>UAB-Histology-00151</peir-vm> | <peir-vm>UAB-Histology-00151</peir-vm> | ||
| − | + | ||
=== Slide 152 Liver and Gallbladder, (H&E) === | === Slide 152 Liver and Gallbladder, (H&E) === | ||
Latest revision as of 23:08, 16 July 2014
Contents
Introduction[edit]
The liver functions as a vast biosynthetic chemical factory, synthesizing large complex molecules from substances brought to it in the blood, particularly substances recently absorbed by the intestine and transported by the portal blood system. All of the biochemical functions of the liver are carried out by the epithelial parenchymal cells of the liver, the hepatocytes. Hepatocytes are responsible for bile synthesis and secretion, excretion of bilirubin, protein carbohydrate and lipid metabolism, storage (vitamins A, D and B12 and iron as ferritin), and conjugation and elimination of metabolites and toxins.
In man the liver consists of 4 lobes. From the surface the right and left lobes are visible and from the visceral surface the caudate and quadrate lobes can be seen. The liver has a fibrous connective tissue covering called the capsule of Glisson. A serosa (= visceral peritoneum) covers the capsule of Glisson in most areas.
The classical hepatic lobule consists of liver parenchyma and anastomosing blood channels, the hepatic sinusoids. The lobules are prismatic or cylindrical in shape, irregularly arranged or distributed throughout the liver, and are about 1 mm wide by 2 mm long. The axis of a lobule is a central vein that receives blood from the hepatic sinusoids and drains into a sublobular vein. The parenchyma of the lobule is organized as broad sheets or plates of cells forming hepatic laminae arranged in a radiating fashion around the central vein like spokes of a wheel. The hepatic sinusoids are irregular blood channels that receive blood from the periphery of a lobule and transport it to the central vein. They separate the hepatic laminae from each other so that one or more surfaces of each hepatocyte are adjacent to a sinusoid.
Blood Supply to a Lobule[edit]
At the periphery of the lobules, in the angles between 2 or 3 adjacent lobules, lie the interlobular septa or portal canals consisting of connective tissue, and containing a branch of the hepatic artery, a branch of the portal vein, a small bile duct, a lymphatic vessel and small nerves. The blood that enters a lobule is supplied from the vessels in the portal system. Both venous and arterial blood enters a lobule. The venous blood enters the sinusoids directly from the smallest branches of the portal vein. Only a small volume of arterial blood enters the sinusoids directly from the smallest branches of the hepatic artery. Most of the arterial blood goes through a capillary bed to enter the small branches of the portal vein before going on to the sinusoids. Blood in the sinusoids “bathes” the hepatocytes before passing into the central vein from which it flows into a sublobular (intercalated) vein. Sublobular veins progressively unite to form the collecting veins that progressively join to form the hepatic veins. Two or more hepatic veins empty directly into the inferior vena cava.
Other details of the liver are given below in conjunction with the microscopic study of the tissue.
Slide 147 Liver, (pig, PASH)[edit]
Scan slide 147 to see how well the lobules are delineated in contrast to the lobular appearance in man. A connective tissue investment surrounds each lobule of the pig liver whereas in man it is much more difficult to see the boundaries of the lobules.
- Find a portal canal in the angles between lobules and identify the "portal triad” i.e., branches of the portal vein, the hepatic artery, and the bile duct. Find a lobule clearly showing the central vein cut in cross section. Under high power observe how the sinusoids are radially arranged around the central vein.
- The hepatic laminae are separated from one another by the sinusoids. The most peripheral lamina or plate of hepatocytes of a lobule is referred to as the limiting lamina.
- Scan the slide with low power to find a lobule in which the central vein is cut in longitudinal section. In such a lobule one can see that the central vein is confluent with a larger vein, the sublobular vein (intercalated vein). Progressive uniting of sublobular veins forms the branches of the hepatic veins. Two or more hepatic veins empty directly into the inferior vena cava.
- The red granulation in the hepatocytes is apparently stored glycogen stained by PAS. Is the glycogen more prevalent in the center or towards the periphery of the lobules, or is there any difference in its distribution?
Slide 152 Liver and Gallbladder and Slide 149 Liver, (H&E)[edit]
The lobules of human liver are not nearly as well defined as in the pig, and it may be difficult to distinguish one clearly. A lobule of the liver contains a central vein as its axis and several portal canals at its periphery. The portal canals are interlobular in position. Find a central vein and follow the sinusoids which radiate from it (actually to it) to the periphery of the lobule. The branching and anastomosing hepatic laminae intervene between the sinusoids.
- Locate a portal canal at the periphery of the lobule and examine its structures. These interlobular areas are not nearly as well defined in human liver as in the pig liver that you have already studied. Identify the branches of the hepatic artery and the portal vein, which is usually the largest structure, found here. The bile duct is lined by low cuboidal to low columnar cells. Small lymphatic vessels are also present. These can probably be identified in the large portal canals. On this slide, the major structures in some of the portal canals may be slightly “unorganized” as a result of postmortem change and histological preparation. The connective tissue in some of the portal areas is slightly infiltrated with lymphocytes.
- In looking over this slide, note that there are blood vessels larger than the central veins coursing independently of the portal canals. The smaller of these are the sublobular veins (= collecting veins; intercalated veins) and the larger are branches of the hepatic vein.
Examine a number of hepatocytes, some of which will be binucleate. The vesicular nuclei show scattered chromatin and one or two nucleoli. The cytoplasm may vary according to the functional state of the cell at the time of fixation.
Pigment granules are sometimes seen in the cytoplasm. These may represent breakdown products of bile.
Vacuolated areas occur more frequently in the cytoplasm where glycogen or fat was dissolved away in preparation of the tissue.
The surface associations of the hepatocyte can be of three types:
- where the cell abuts next to an adjacent cell;
- where the surface is slightly separated from an adjacent cell to form the lumen of a bile canaliculus;
- an external surface adjacent to a perisinusoidal space (space of Disse).
Study the sinusoids. These intralobular vascular blood channels, averaging 9 to 12 μm's in diameter, converge to form the central vein. Two main types of cells (endothelial cells and the phagocytic stellate cells of Kupffer) form the lining of the sinusoid, and a third cell type, the fat storing cell, is located in the perisinusoidal spaces. This latter cell is not evident on our slide.
The endothelium forming most of the sinusoidal lining is not continuous; rather, the margins of adjacent endothelial cells may either have typical junctions, or they can be discontinuous in which the adjacent cell margins are separated by a space of 100 nm to 500 nm. A basal lamina is absent, but the cells are probably supported by reticular fibers.
The phagocytic cells, known as stellate cells or Kupffer cells are situated on the endothelium or they actually form part of the sinusoidal lining. Processes of these macrophages often extend between the endothelial cells and across the sinusoidal lumen. Their changing shape may show varied relationships to the endothelial cells. The stellate cells are replenished by mitosis and from the circulating monocyte pool.
On this slide the stellate cells are best identified by their oval, large nucleus with delicate chromatin and one nucleolus (not prominent). Their branching pseudopodial cytoplasmic processes can often be distinguished. The best way to demonstrate Kupffer cells is to inject a vital dye into an animal before fixation of the livers.
The endothelial cell is smaller and more flattened than the stellate cell. It has a small, dark ovoid nucleus and the cytoplasm is highly attenuated. EM photographs of the endothelial cells show large variable-sized fenestrae in the cytoplasm. The fenestrae or “pores” are oval-shaped and they average about 100 nm in diameter.
Between the hepatocyte and the sinusoid is a fluid-filled space (or potential space) known as the perisinusoidal space (space of Disse). Identify several on your slide. Microvilli project from the free surfaces of the hepatocytes into this space. Chylomicrons and blood plasma pass through the gaps between endothelial cells and through the fenestrated cytoplasm to gain access to the perisinusoidal space to come in contact with the hepatocyte surface.
Lymph produced by the liver is believed to flow in the perisinusoidal space towards the periphery of a lobule. At the periphery it percolates into the interstitial spaces in the connective tissue of the portal canal from which it passes into lymphatic capillaries. No direct connections occur between the lymphatic capillaries and the perisinusoidal spaces. Silver stains demonstrate a network of reticular fibers forming a framework that surrounds each sinusoid. This framework occupies the perisinusoidal space lying between the hepatocytes and the sinusoidal lining.
Bile is the exocrine serous fluid secreted (excreted) by the liver. It is elaborated by the hepatocytes and transported to the periphery of a lobule by way of the intercellular bile canaliculi. A canaliculus does not have a wall or epithelium of its own. Instead, canaliculi are formed between the plasma membranes of two adjacent hepatocytes. The canaliculus is formed by a “matched pair of grooves on facing cell membranes.” At the interface of the two cells the plasma membranes separate to form an intercellular canal or bile canaliculus measuring 0.5 to 1.5 μm in diameter. A zonula occludens occurs at each side of the lumen of the canaliculus. Farther away from the lumen may be a zonula adherens (not consistently present) and/or a macula adherens (desmosome). At the ultrastructural level, microvilli are seen to protrude into the lumen of the canaliculus.
Bile canaliculi will be difficult to identify on this section, but you should look for them. Remember, they range from 0.5 to 1.5 μm in diameter!
Leading from the bile canaliculi at the periphery of a lobule are small bile ductules called cholangioles (canals of Hering) which unite the intralobular canaliculi with the interlobular bile ducts. These tiny ductules have a low cuboidal epithelium and a lumen hardly larger than that of a bile canaliculus. It will take diligent searching to find one on your slide.
In some portal areas you may see large bile ducts which are lined by simple high columnar cells and have a connective tissue investment. The larger of these branches in the liver unite to form the right and left hepatic ducts that in turn join to form the hepatic duct. The cystic duct of the gallbladder and the hepatic duct join to form the common bile duct.
Remember that lymph and bile flow from a lobule in a direction opposite to the flow of blood in the sinusoids.
Slide 152, Liver and Gallbladder (H&E)[edit]
Slide, 149 Liver (H&E)[edit]
Gallbladder[edit]
The pear-shaped gallbladder shows marked variation in size and shape among different individuals. Anatomically, it consists of a neck, a body, and a blindly ending fundus. Histologically, its wall consists of a mucosa, a muscularis, a perimuscular layer of connective tissue, and a serosa or fibrosa.
Slide 151 Gallbladder, (H&E)[edit]
Mucosa - The mucosa consists of an epithelium, its basement membrane, and an underlying lamina propria of loose connective tissue. The tall, simple columnar epithelial cells of the mucosa are absorptive in nature. They have basal ovoid nuclei and on their luminal surface is a thin striated border (demonstrated by EM). No goblet cells are present in this epithelium. The mucosa of the non-distended gallbladder is irregularly folded, somewhat resembling villi when it is sectioned. These folds largely disappear when the gallbladder is filled.
Simple tubuloalveolar glands exist only in the neck region of the gallbladder, but none are present on our slides. The “hollowed out” epithelial-lined “pockets” which you may see on your slides represent blind recesses or diverticula of the folded epithelium that have been sectioned; they are not glands. The lamina propria is a delicate loose connective tissue containing many small blood vessels. Occasionally, one can see a few smooth muscle fibers scattered within it, but a muscularis mucosae is lacking. The gallbladder also lacks a submucosa.
Muscularis - The smooth muscle of the muscularis forms interlacing and somewhat irregular bundles that may be cut longitudinally, transversely or obliquely. A fibroelastic network accompanies the muscle bundles.
Perimuscular layer - External to the muscularis is the perimuscular layer of irregular connective tissue through which course the large blood vessels, nerves, and lymphatics that supply the organ. Here may be found collagenous and elastic fibers, fibroblasts, wandering lymphocytes, macrophages, fat cells and occasional small ganglia.
Serosa or fibrosa - The outermost layer of the free surface of the gallbladder is serosa (visceral peritoneum); it may be torn off the section. Where the gallbladder attaches to the liver, a fibrosa is present (seen on slide 152).
Slide 152 Liver and Gallbladder, (H&E)[edit]
Portal canals and central veins show variations in size and are particularly well preserved.
- The continuity of the sinusoidal lumens with the lumen of the central vein can be observed in many areas.
- Several portal canal areas exhibit lymphocytic infiltration.
- Hepatocytes are well preserved; many are binucleate.
- Stellate cells (Kupffer cells) with visible cytoplasm and delicate cell processes can be observed. These should be distinguished from the endothelial cells lining the sinusoid.
Several portal vein branches are present in association with larger branches of the hepatic artery and bile duct (large portal canals).
A portion of the gallbladder is attached to the liver.
Study the serosa of the liver and its relation to the serosa of the gallbladder. Is the serosa continuous?
Identify the layers of the gallbladder.
Observe the area between the liver and gallbladder. This outer connective tissue layer of the gallbladder where it attaches to the liver is called the fibrosa; it merges with the connective tissue capsule of the liver.
The simple columnar epithelium of the gallbladder is highly absorptive and is well preserved in this section.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
A bladder diverticulum is an out-pouching of the bladder wall, usually caused by chronic urethral obstruction.