Difference between revisions of "Histologic:Chapter 16"
(→The Testis) |
Seung Park (talk | contribs) (→Slide 284, Penis (H&E)) |
||
| (One intermediate revision by one other user not shown) | |||
| Line 125: | Line 125: | ||
=== Prostate Gland === | === Prostate Gland === | ||
| − | + | [[File:HistologicChapter16Prostate.jpg|thumb|200px|Prostate]] | |
The prostate gland is an accessory, unpaired sex gland of males that surrounds the urethra as it leaves the bladder. The prostate is an aggregation of 30 to 50 branched tubuloalveolar glands that secrete a milky fluid rich in citric acid and acid phosphatase. Grossly, the prostate gland has five lobes and is about one and a half inches in diameter. It is surrounded by a fibromuscular capsule. | The prostate gland is an accessory, unpaired sex gland of males that surrounds the urethra as it leaves the bladder. The prostate is an aggregation of 30 to 50 branched tubuloalveolar glands that secrete a milky fluid rich in citric acid and acid phosphatase. Grossly, the prostate gland has five lobes and is about one and a half inches in diameter. It is surrounded by a fibromuscular capsule. | ||
| Line 213: | Line 213: | ||
For most of its length the penile urethra is lined by non-secreting columnar epithelium into which small mucus glands embedded in the corpus spongiosum drain. Within the glans penis, however, the urethra dilates (navicular fossa) and becomes lined by non-keratinizing stratified squamous epithelium identical to that covering the glans. | For most of its length the penile urethra is lined by non-secreting columnar epithelium into which small mucus glands embedded in the corpus spongiosum drain. Within the glans penis, however, the urethra dilates (navicular fossa) and becomes lined by non-keratinizing stratified squamous epithelium identical to that covering the glans. | ||
| − | + | ||
| + | |||
<peir-vm>UAB-Histology-00284</peir-vm> | <peir-vm>UAB-Histology-00284</peir-vm> | ||
Latest revision as of 23:39, 28 July 2014
Introduction[edit]
The components of the male reproductive system include the testes, the genital ducts, the accessory glands, and the penis.
The Testis[edit]
The testis functions as a cytogenic gland in that it produces spermatozoa and as an endocrine gland which produces the hormone testosterone. This hormone is essential for the proper development and maintenance of the accessory sexual organs, particularly the genital ducts and the accessory glands.
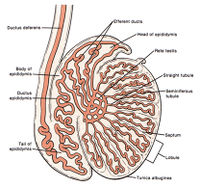
The two ovoid testes lie in the scrotum. Each testis is covered by three tunics.
- A prominent, tough, fibrous layer of connective tissue called the tunica albuginea forms the middle tunic.
- Investing the tunica albuginea is a layer of squamous cells and a thin layer of loose connective tissue, the tunica vaginalis, which represents a serous lining of peritoneum “trapped” by the descended testis. This tunic is lacking on the posterior wall of the testis.
- Internal to the tunica albuginea is a thin layer of loose, highly vascular connective tissue called the tunica vasculosa.
The testis is divided into about 250 anastomosing, pyramidal-shaped lobules by delicate connective tissue septa, the septulae testis. The septa radiate from the mediastinum into the testis. Within the testicular lobules occur from one to four convoluted seminiferous tubules where spermatozoa are produced.
The stroma of the testis lies between the seminiferous tubules. In addition to the usual connective tissue cells and collagenous fibers found in loose, vascular connective tissue, the stroma also contains endocrine tissue consisting of the interstitial cells (cells of Leydig). These cells produce the androgenic steroid hormone testosterone. Production of testosterone is stimulated by luteinizing hormone (LH = interstitial cell stimulating hormone, ICSH) produced by basophils of the anterior pituitary gland. Interstitial cells are polyhedral shaped cells (14 to 21 μm in diameter) with a large, rounded, sometimes wrinkled nucleus, and an acidophilic cytoplasm. The cytoplasm, in addition to the usual organelles, also contains a vast amount of smooth endoplasmic reticulum and mitochondria containing tubular cristae. These organelles are characteristic of cells which produce steroid hormones. Another cytoplasmic characteristic of interstitial cells are protein crystals (of Reinke) that vary in size, form and frequency of occurrence. The significance of these crystals is not clear.
A seminiferous tubule has a highly complex stratified epithelium consisting of spermatogenic cells and supporting cells (= sustentacular or Sertoli cells). External to the basement membrane on which the epithelium rests is a tunic of fibroelastic tissue. The supporting cells are tall, irregular columnar cells extending from the basement membrane to the lumen of the seminiferous tubule. On the lateral and apical surfaces, numerous recesses are formed by the plasma membrane which “indents” the cytoplasm. Within these recesses or depressions lie developing spermatogenic cells. The elaborate shapes of the supporting cells are difficult to see unless the testis has been prepared by a silver technique which demonstrates the cell boundaries. The large nuclei (9 to 12 μm diameter) of supporting cells have a variable position ranging from the basal zone to the mid- region of the cell. The nucleus is usually ovoid, stains palely, and shows an unusual tripartite nucleolus possessing a central acidophilic mass flanked by two basophilic masses. The nuclear membrane is frequently folded or longitudinally indented. The presence of moderate amounts of smooth endoplasmic reticulum and other features characteristic of steroid producing cells have led to suggestions that the supporting cells may produce steroid hormones. The major role of these cells is in mechanical support, protection, and perhaps nourishment of the developing germ cells.
Slide 227, Testis (H&E)[edit]
Scan this slide to observe:
Section of testis containing sections of seminiferous tubules. Note the dense tunica albuginea, the tunica vasculosa, the septula testis and the connective tissue stroma or interstitial tissue.
Identify the mediastinum testis containing the irregular channels of the rete testis.
A portion of the epididymis is present (the mass of tissue at one end) and can be seen containing efferent ducts and sections of the ductus epididymis. The former are in the uppermost area, the latter in the lowermost region.
Note the numerous blood vessels, nerves and abundance of connective tissue fibers and adipose tissue adjacent to the mediastinum and epididymis.
Study the normal seminiferous tubules. Locate the three layers that constitute the wall of a tubule. These are:
- An outermost layer of fibroelastic connective tissue.
- A basement membrane on which the spermatogonial and supporting cells rest.
- The complex stratified epithelium where spermatogenesis occurs.
The three layers may be seen more easily on slide 228, Testis (Masson) where the basement membrane is stained blue.
On slide 227, 228 and 230 identify the interstitial cells in the stromal tissue lying in angles between the seminiferous tubules. Interstitial cells are polyhedral in shape, have an acidophilic cytoplasm, and possess a rounded nucleus that usually contains one or two prominent nucleoli. The cytoplasm may be vacuolated where lipid droplets were dissolved away and an occasional cell may contain golden brown deposits of lipochrome pigment.
On the same slides, identify the supporting cells (Sertoli cells) within the stratified epithelium of the seminiferous tubules. Their cell boundaries will not be seen, but one usually can identify the nuclei of these tall columnar cells. The ovoid nucleus stains palely, contains a nucleolus and will occupy a variable position ranging from near the basement membrane to the middle of the cell.
Within the seminiferous tubules of slide 230 identify as many of the spermatogenic cells as possible.
Slide 228, Testis (Masson)[edit]
Slide 230, Testis[edit]
Genital Ducts[edit]
Straight tubules. On slide 227, Testis (H&E) identify the straight tubules located in a narrow region between the ends of the seminiferous tubules and the rete testis. The simple columnar epithelial cells, which line the initial segment of the straight tubules, resemble supporting cells. Near the rete testis the cells shorten to become cuboidal. These tubules have a uniformly narrow diameter.
Rete testis. The rete testis is located in the connective tissue of the mediastinum testis. It is that portion of the genital ducts which unites the straight tubules (tubuli recti) with the efferent ducts. The rete testis is essentially a system of anastomosing channels of epithelial lined spaces within connective tissue. As such the epithelium of these irregular spaces consists of low simple cuboidal to simple squamous cells resting on a basement membrane. A single cilium may occur on some of the cells. (Not seen on our slide.) A distinct lamina propria and muscularis are lacking. On slides 227 and 230 locate and study the rete testis in the dense connective tissue of the mediastinum. On these slides, its extent varies from extensive to virtually absent.
Efferent ducts. Efferent ducts (ductuli efferentes). About twelve to fifteen ductules (0.6 mm in diameter, 4 to 6 mm long) called efferent ducts unite the rete testis with the ductus epididymis. The ductules emerge from the mediastinum to the surface of the testis where they form cone-shaped coils that constitute much of the head of the epididymis. The efferent ducts consist of an epithelium resting on a thin basement membrane and some circularly oriented smooth muscle fibers embedded within the connective tissue surrounding the ductules.
On slide 227, Testis (H&E), and slide 230, Testis, (H&E) locate the efferent ducts in the epididymal region by the scalloped or undulated appearance of the epithelium. They appear in the lower right field on slide 227 and in the upper right field on slide 230. The epithelium is pseudostratified with small basal cells near the basement membrane and larger columnar or cuboidal surface cells. This gives the luminal surface of the ducts an irregular contour. The columnar cells are usually ciliated, whereas microvilli extend into the lumen from the cuboidal cells. (Cilia and microvilli are difficult to see on our slide.) Transport of sperm to the ductus epididymis is facilitated by the beating of the cilia. Motile cilia in the male genital ducts are found here and in the rete testis. The microvilli probably serve an absorptive function. Pigment granules and pale secretion granules may sometimes be seen in both types of surface cells of the ducts. Also, clear areas occur within the cells where fat has been dissolved away. On the upper right edge of slide 230 is a long, cystic tubule, probably an efferent duct that became obstructed.
Ductus epididymis. The epididymis lies on the posterior side of the testis. The ductus epididymis consists of a highly coiled duct (or tube) five to six meters in length, surrounded by smooth muscle and connective tissue. It occupies the body and the tail of the epididymis. The ductus epididymis unites proximally with the efferent ducts and distally with the ductus deferens. The duct is lined with a pseudostratified columnar epithelium consisting of tall columnar cells and smaller rounded basal cells. Large, nonmotile, branching microvilli called stereocilia extend from the apices of the columnar cells. Within the cytoplasm of these cells are secretory granules or vacuoles and pigment. Surrounding the epithelium is a thin lamina propria encircled by a very thin layer of smooth muscle. Outside the smooth muscle lies loose to compact connective tissue that forms the interstitium or stroma of the epididymis.
Slide 229, Ductus Epididymis (Masson)[edit]
Observe:
That numerous coils of the duct have been sectioned in various planes.
The relatively smooth lumen of the duct, owing to the uniform thickness of the epithelium and the stereocilia extending into the lumen.
The sperm stored within the lumen.
The scant amount of stromal connective tissue and smooth muscle surrounding the various coils of the duct.
Slide 6, Ductus Epididymis (H&E)[edit]
Note especially the pseudostratified columnar epithelium possessing tall stereocilia.
Slide 230, Testis (H&E)[edit]
Study slide 230, Testis (H&E) for comparison of efferent ducts and ductus epididymis.
Locate the numerous sections of the ductus epididymis (lower right field in both slides). Again, note the relatively smooth outline of the luminal surface of the ductus epididymis. Compare the appearance of this duct with the scalloped appearance of the efferent ducts previously studied on these slides (in the upper fields) especially on slide 230 where the latter are more numerous.
Ductus deferens. During development the testis descends from its early position on the posterior abdominal wall into the pelvis, and later during the seventh month of fetal life, it passes through the inguinal canal into the scrotum. Upon descending, each testis “pulls along” its vessels, nerves and ducts (ductus deferens) with it. These structures constitute the spermatic cord. The components of the spermatic cord are surrounded by connective tissue layers (fascia of gross anatomy) and by a somewhat discontinuous, longitudinally oriented layer of striated muscle fibers of the cremaster muscle.
The constituents of the spermatic cord are the:
- ductus deferens
- artery of the ductus deferens
- testicular artery
- cremasteric artery
- pampiniform plexus of veins
- lymphatic vessels
- nerves of the testis and epididymis
Slide 232, Spermatic Cord (H&E)[edit]
Scan the tissue to observe:
- The large ductus deferens with its thick muscular coat.
- The numerous veins which constitute the pampiniform plexus. Some of these veins have unusually thick muscular tunics and bundles of longitudinally oriented muscle in the adventitia (medium-sized veins).
- Arteries
- Nerves
- Connective tissue fibers and adipose tissue of the fascial layers.
Accessory Glands[edit]
Prostate Gland[edit]
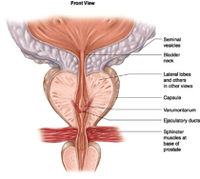
The prostate gland is an accessory, unpaired sex gland of males that surrounds the urethra as it leaves the bladder. The prostate is an aggregation of 30 to 50 branched tubuloalveolar glands that secrete a milky fluid rich in citric acid and acid phosphatase. Grossly, the prostate gland has five lobes and is about one and a half inches in diameter. It is surrounded by a fibromuscular capsule.
The individual glands making up the overall prostate are arranged into a mucosal, a submucosal, and a main group of glands. They lie embedded in a fibromuscular stroma. The prostatic urethra traverses the prostate gland from superior to inferior surfaces. On each side of the prostatic utricle (the male homologue to the vagina) are located the ejaculatory ducts which open into the prostatic urethra. The ejaculatory ducts and the prostatic utricle are located in the seminal colliculus, an elevated portion of the urethral crest. The urethral crest is a longitudinal ridge that forms the posterior wall of the prostatic urethra.
Slide 123, Prostate (H&E)[edit]
Study Slide 123, Prostate (H&E) which is a section of the prostate from a 26- year-old male. Under low power note the numerous glands surrounded by the fibromuscular stroma. These glands are from the main group of glands of the prostate. Study them for detail noting that:
The epithelium is low pseudostratified, having columnar cells and basal cells resting on a thin basement membrane (not seen here). The apices of the columnar cells appear “washed out” (poorly stained) indicating that some of the secretory material has been lost in fixation and/or that the secretory droplets stain poorly with H&E. The apices of most of the secretory cells stain positively with lipid stains.
The epithelium shows numerous folds. Some of the folds have been sectioned tangentially and here the epithelium appears stratified. In other areas, the folds are cut through and appear as small “isolated islands” of epithelium.
Eosinophilic prostatic concretions (corpora amylacea) can be seen within the lumina of the glands. These rounded bodies increase with age following adulthood. They contain carbohydrate and protein and may become large enough to occlude the lumens of the glands. When calcified they are called calculi.
Study the abundant fibromuscular stroma making up about one-fourth to one-third of the gland. Strands of smooth muscle varying in thickness are intermixed with collagenous and elastic fibers. The muscle does not appear to have definite orientation or layers. This fibromuscular stroma is a distinctive feature of the prostate.
Slide 124, Prostatic Urethra (H&E)[edit]
On slide 124, Prostatic Urethra (H&E), the general distribution of the somewhat concentrically arranged mucosal, submucosal and main prostatic glands can be studied. Identify these glands according to their locations.
The mucosal glands are smallest and are periurethral in position (next to the urethra). Their ducts open at various points into the urethra. (These are small, few in number and may be absent on your section.)
The submucosal glands are immediately peripheral to the mucosal ones, and the main glands which are largest and most numerous, lie to the outside of the submucosal glands on the periphery of the section. The ducts of the submucosal and main glands open into the urethral sinuses.
Abnormalities are present. Some of the main glands show cystic dilations.
The epithelium of these cystic glands is less folded than in the normal glands and in some regions appears to be squamous and less secretory than normal. Some glands may show lymphocytic infiltration. Others have stratified epithelium (hyperplasia).
Study the prostatic urethra, a U-shaped groove in the prostate, and the urethral crest, a longitudinal ridge that forms the posterior wall of the prostatic urethra. The posterolateral portions of the urethra on each side of the urethral crest are the urethral sinuses. It is here where the ducts of the submucosal and main glands empty secretions into the urethra.
Note the epithelium of the urethra. It is usually classified as transitional epithelium but patches of stratified columnar epithelium may be present.
Most slides do not have ejaculatory ducts or the prostatic utricle since the section was taken through the prostate superior to the entrance of these structures into the urethra, but parts of these two structures may be present. The part of the urethral crest in which the prostatic utricle is located is the colliculus seminalis.
Observe the periurethral vascular supply and the venous plexuses in the urethral crest.
Seminal Vesicles[edit]
The seminal vesicles are paired saccular organs each in the form of a convoluted tube. They lie posterior to the prostate and their secretions, rich in fructose, enter the ejaculatory ducts just below the ampulla of the ductus deferens. The three layers of the gland are a mucosa, a muscularis and an adventitia (= fibrosa). The single lumen is irregular and branching with numerous lateral outpocketings.
Slide 237, Seminal Vesicle (H&E)[edit]
Observe that the gland appears to possess numerous lumina. Actually only one continuous cavity is present, but when the numerous convolutions of the gland are cut in one plane, separate cavities appear to be present.
Note the complicated folding of the mucosa in which thin primary folds often exhibit secondary and tertiary branching.
The muscularis contains an inner circular and an outer longitudinal layer of smooth muscle; two layers are not easily distinguishable in a section.
The adventitia or fibrosa is rich in elastic fibers. It contains large blood vessels, nerves, and blends with other connective tissue surrounding the gland. One or more ganglia may be present.
With high power study the mucosa on slide 237. The epithelium may appear to be simple cuboidal or low columnar, but the presence of basal cells makes it a low pseudostratified epithelium. The lining cells are secretory. A few granules may be present, or vacuoles may occur where they were dissolved away. Look for yellow or brownish lipochrome pigment in the surface cells. This pigment gives a yellowish tinge to the viscid secretions coming from these glands. The pigment begins to appear at puberty and increases with age. Beneath the epithelium is a basement membrane and a thin lamina propria with abundant elastic fibers.
Bulbourethral Gland[edit]
Slide 238, Bulbourethral Gland (Masson)[edit]
Scan Slide 238, Bulbourethral gland (Masson) to observe that:
The irregular lobules of this compound tubuloalveolar gland are separated from each other by connective tissue septa that extend inward from a thin capsule.
At the periphery of the gland and also in the connective tissue septa between some of the lobules can be seen skeletal muscle fibers.
Interlobular excretory ducts lie within some of the larger connective tissue septa. (See e below)
With high power study the parenchyma consisting of pale secretory cells, usually cuboidal to columnar in shape. They resemble mucous cells. The nucleus tends to be flattened at the base of the cells; however, some are rounded, others are oval and vertically oriented. The varying shapes of the nuclei probably indicate different states of secretory activity exhibited by the cells at the time of fixation. A mucus-like discharge from these glands lubricates the urethra during sexual simulation.
In the smaller ducts of the bulbourethral gland the epithelium is simple and quite variable ranging from low cuboidal to columnar. The large excretory ducts are lined by stratified columnar epithelium that may contain patches of secreting cells. Smooth muscle fibers can usually be found among the connective tissue fibers surrounding these ducts and also in other regions of the connective tissue septa.
Penis[edit]
Slide 284, Penis (H&E)[edit]
The penis is composed of erectile tissue and contains the section of penile urethra. The erectile tissue is composed of two dorsal cylinders (corpora cavernosa) and a smaller central ventral cylinder (corpus spongiosum) through which the penile urethra runs. These cylinders are each surrounded by a dense fibrocollagenous sheath, the tunica albuginea. The erectile tissues are essentially interconnecting vascular spaces which are empty when the penis is flaccid but which become engorged with blood during an erection.
The blood supply to the penis is provided by the dorsal and the deep arteries. From the deep arteries arise arteries supplying the tunica albuginea, and the helicine arteries, which supply the erectile tissue. The helicine arteries form convoluted vessels in the flaccid penis but during erection they straighten and dilate, filling the corpora with blood. This filling effect is partly due to closure of the arteriovenous shunts existing between the helicine arteries and deep veins, which constitute the normal route of helicine artery blood flow in the flaccid state. Parasympathetic nerve discharges cause the closure, leading to diversion of the helicine artery blood into the cavernous spaces, while increased pressure in the corpora compresses the thin-walled veins, preventing emptying. After ejaculation the parasympathetic stimulation ceases, the arteriovenous shunts open and blood passes from the corpora into the veins.
At the distal end of the penis the corpus spongiosum terminates on the glans penis, which is covered with non-keratinizing squamous epithelium containing sebaceous glands. The penile urethra opens to the exterior at the meatus at the centre of the glans penis
For most of its length the penile urethra is lined by non-secreting columnar epithelium into which small mucus glands embedded in the corpus spongiosum drain. Within the glans penis, however, the urethra dilates (navicular fossa) and becomes lined by non-keratinizing stratified squamous epithelium identical to that covering the glans.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
A normal partial thromboplastin time is 28 to 37 seconds.
Corpora amylacea are small hyaline masses of degenerated cells and inspissated secretions. They are so named because they resemble (but are categorically not) amyloid deposits.