Difference between revisions of "IPLab:Lab 7:IDC"
Seung Park (talk | contribs) |
Seung Park (talk | contribs) |
||
| Line 16: | Line 16: | ||
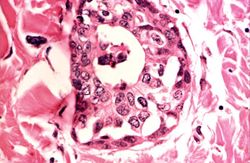
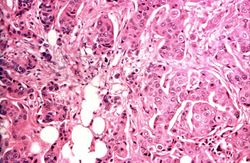
File:IPLab7IDC8.jpg|This is a high-power photomicrograph demonstrating the growth pattern of the tumor. The tumor consists of malignant duct-lining cells growing in cords, solid cell nests, tubules, and glands. The cytologic detail of tumor cells varies from small cells with moderately hyperchromatic, regular nuclei to large cells with large, irregular, hyperchromatic nuclei. | File:IPLab7IDC8.jpg|This is a high-power photomicrograph demonstrating the growth pattern of the tumor. The tumor consists of malignant duct-lining cells growing in cords, solid cell nests, tubules, and glands. The cytologic detail of tumor cells varies from small cells with moderately hyperchromatic, regular nuclei to large cells with large, irregular, hyperchromatic nuclei. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="What is the most common type of breast tumor?">Invasive ductal carcinoma is the most common type of breast tumor, accounting for 65 to 80% of all mammary cancers.</spoiler> | ||
| + | * <spoiler text="Are the fibroblasts that make up the desmoplasia seen in infiltrating duct carcinomas neoplastic?">No, the dense fibrous connective tissue is a reaction to the neoplastic epithelial cells.</spoiler> | ||
| + | * <spoiler text="What factors predispose to breast cancer?"># Geographic influences: Five times more common in the United States than in Japan and Taiwan. | ||
| + | # Genetic predisposition: The risk is 1.5 to 2 times for women with one first-degree relative with breast cancer, 4 to 6 times for those with two affected relatives. There are uncommon high-risk families with apparent autosomal dominant transmission and familial association of breast and ovarian carcinomas. Breast cancer affects 25% of patients with the Li-Fraumeni syndrome (multiple sarcomas and carcinomas), which, is associated with germ-line mutations of the tumor suppressor gene p53. | ||
| + | # Increasing age: Uncommon before age 25, but then a steady rise to the time of menopause, followed by a slower rise throughout life. | ||
| + | # Length of reproductive life: Risk increases with early menarche and late menopause. | ||
| + | # Parity: More frequent in nulliparous than in multiparous women. | ||
| + | # Age at first child: Increased risk when older than 30 years of age at time of first child. | ||
| + | # Obesity: Increased risk attributed to synthesis of estrogens in fat depots. | ||
| + | # Exogenous estrogens: Moderately increased risk with high-dosage therapy for menopausal symptoms. | ||
| + | # Oral contraceptives: No clear-cut increased risk; attributed to balanced content of estrogens and progestins in currently used oral contraceptives. | ||
| + | # Fibrocystic changes with atypical epithelial hyperplasia: Increased risk, as noted in earlier discussion of this condition. | ||
| + | # Carcinoma of the contralateral breast or endometrium: Increased risk.</spoiler> | ||
| + | * <spoiler text="What are the most important prognostic factors for patients with breast cancer?"># The size of the primary tumor, tumors of less than 2 cm being associated with favorable prognosis. | ||
| + | # Lymph node involvement and the number of lymph nodes exhibiting metastases. | ||
| + | # The histologic type and grade of tumor. The survival rate for intraductal carcinoma is 74%; for papillary carcinoma, 65%; for medullary carcinoma, 58%; for colloid, 58%; for infiltrating lobular, 34%; and for infiltrating ductal, 29%. | ||
| + | # The presence or absence of estrogen and progesterone receptors. The highest response rates are in patients with tumors containing both estrogen and progesterone receptors. On the whole, cancers with high levels of estrogen receptors have a better prognosis than those with intermediate levels or no receptors. | ||
| + | # The proliferative rate of the tumor and aneuploidy. | ||
| + | # The presence of amplified or activated oncogenes, particularly c-erbB2 in tumor tissue. | ||
| + | # The degree of angiogenesis in the tumor. | ||
| + | # The presence of enzymes, such as cathepsin D and stromelysin, which are involved in tumor invasion. | ||
| + | |||
| + | Overall, axillary node status is the single most important prognostic factor for patients with early breast cancer. However, 20 to 30% of patients with histologically negative lymph nodes will suffer recurrences and die of their disease within 10 years.</spoiler> | ||
{{IPLab 7}} | {{IPLab 7}} | ||
[[Category: IPLab:Lab 7]] | [[Category: IPLab:Lab 7]] | ||
Revision as of 15:33, 21 August 2013
Clinical Summary[edit]
This 66-year-old female had had a mass of increasing size in the left breast for many years. A modified radical mastectomy was performed. At that time, invading carcinoma was left around the subclavian artery and 9 of 9 axillary lymph nodes were found to contain metastases. Later, pleural effusions recurred despite radiation therapy. The patient died 3 months after surgery.
Autopsy Findings[edit]
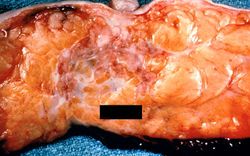
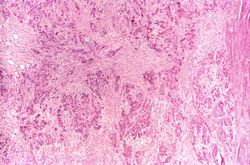
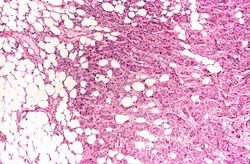
The left breast was large (1700 grams), measuring 34 x 22 x 7 cm. A very large tumor involving all quadrants and measuring about 14 cm in diameter was noted. The nipple and skin were involved, the latter showing the typical orange peel appearance. On section, virtually the entire breast was replaced by a tumor composed of firm, yellowish-white tissue. Extension into the fatty tissue and to the skin was evident grossly.
Images[edit]
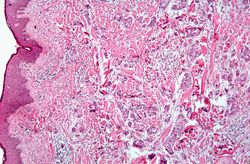
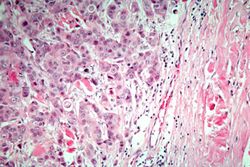
This is a high-power photomicrograph demonstrating the growth pattern of the tumor. The tumor consists of malignant duct-lining cells growing in cords, solid cell nests, tubules, and glands. The cytologic detail of tumor cells varies from small cells with moderately hyperchromatic, regular nuclei to large cells with large, irregular, hyperchromatic nuclei.
Study Questions[edit]
A radical mastectomy involves removal of the breast, underlying pectoralis muscles, and axillary lymph nodes.
Pleural effusion is the presence of fluid in the pleural space. Increased hydrostatic pressure in the pulmonary vasculature, as seen in heart failure, is one cause of pleural effusion.
An infiltrate is an accumulation of cells in the lung parenchyma--this is a sign of pneumonia.