Difference between revisions of "IPLab:Lab 6:Hashimoto's Thyroiditis"
(→Autopsy Findings) |
(→Images) |
||
| Line 7: | Line 7: | ||
<gallery heights="250px" widths="250px"> | <gallery heights="250px" widths="250px"> | ||
File:IPLab6Hashimoto1.jpg|This is a gross photograph of thyroid gland taken at autopsy. The gland is only slightly enlarged and has a firm texture. | File:IPLab6Hashimoto1.jpg|This is a gross photograph of thyroid gland taken at autopsy. The gland is only slightly enlarged and has a firm texture. | ||
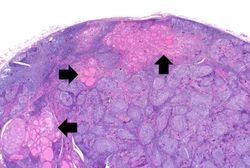
| − | File: | + | File:IPLab6Hashimoto3.jpg|This is a low-power photomicrograph of thyroid from this case. Note the large number of blue-staining inflammatory cells in this tissue. These blue cells appear to be forming germinal centers. Some residual thyroid gland tissue can be seen in this section (arrows). |
| − | |||
| − | |||
File:IPLab6Hashimoto5.jpg|This is a higher-power photomicrograph of thyroid from this case showing the inflammatory cells and the residual thyroid tissue. | File:IPLab6Hashimoto5.jpg|This is a higher-power photomicrograph of thyroid from this case showing the inflammatory cells and the residual thyroid tissue. | ||
| − | |||
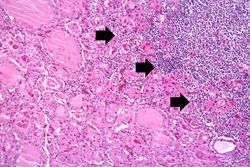
File:IPLab6Hashimoto7.jpg|This is a high-power photomicrograph showing the inflammatory cells infiltrating into the residual thyroid tissue (arrows). | File:IPLab6Hashimoto7.jpg|This is a high-power photomicrograph showing the inflammatory cells infiltrating into the residual thyroid tissue (arrows). | ||
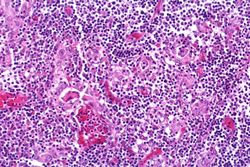
File:IPLab6Hashimoto8.jpg|This is a high-power photomicrograph showing the lymphocytes and plasma cells surrounding the thyroid gland epithelium. | File:IPLab6Hashimoto8.jpg|This is a high-power photomicrograph showing the lymphocytes and plasma cells surrounding the thyroid gland epithelium. | ||
| − | |||
</gallery> | </gallery> | ||
Revision as of 23:26, 8 July 2020
Contents
Clinical Summary[edit]
This was a 49-year-old woman who complained of tiredness and difficulty concentrating. She had gained weight over the last year and despite warm weather, she felt chilled without a sweater. Family history was significant for hypothyroidism in her mother and older sister.
On physical examination she had an enlarged thyroid gland with a firm, bosselated texture. Serum TSH was markedly elevated and antithyroid peroxidase antibodies were positive. These results supported the clinical impression of hypothyroidism; also, the texture of her thyroid gland and a positive family history suggested an autoimmune etiological factor. She was referred to an endocrinologist; however, before beginning treatment she died suddenly from a ruptured berry aneurysm.
Images[edit]
Virtual Microscopy[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Hashimoto Thyroiditis
- eMedicine Medical Library: Hypothyroidism
- Merck Manual: Overview of Thyroid Function
- Merck Manual: Hashimoto's Thyroiditis
- Merck Manual: Hypothyroidism
Journal Articles[edit]
- Agrawal P, Ogilvy-Stuart A, Lees C. Intrauterine diagnosis and management of congenital goitrous hypothyroidism. Ultrasound Obstet Gynecol 2002 May;19(5):501-5.
Images[edit]
Related IPLab Cases[edit]
Bosselated means covered with rounded protuberances.
Autoimmune disorders involve an immune response directed at the host's own cells.
A berry aneurysm is a small saccular arterial aneurysm usually found at a vessel junction in the circle of Willis. These aneurysms frequently rupture, causing a subarachnoid hemorrhage.