Difference between revisions of "IPLab:Lab 6:Glomerulonephritis"
Seung Park (talk | contribs) (→Journal Articles) |
(→Autopsy Findings) |
||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
== Clinical Summary == | == Clinical Summary == | ||
| − | This | + | This 27-year-old male had end-stage renal disease requiring hemodialysis for 10 years. For the previous four years he had hypertension which slowly increased to about 180/120 mm Hg. Laboratory findings included a markedly elevated BUN and creatinine. He underwent bilateral nephrectomy and was placed on the transplant list. |
| − | + | On examination the kidneys were similar in appearance. Cortices were pale, diffusely granular with a few 1-2 mm cysts. On being sectioned, the cortex of each kidney was thin (4-5 mm) and pale. Renal medullae were pale yellow-tan in color and there was abundant peripelvic fat. The ureters, pelvis, calyces and hilar vessels showed no abnormalities. | |
| − | |||
== Images == | == Images == | ||
| Line 18: | Line 17: | ||
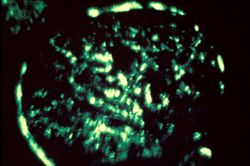
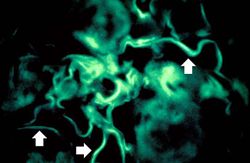
File:IPLab6GN10.jpg|For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome. | File:IPLab6GN10.jpg|For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Virtual Microscopy == | ||
| + | <peir-vm>IPLab6GN</peir-vm> | ||
== Study Questions == | == Study Questions == | ||
| Line 37: | Line 39: | ||
=== Images === | === Images === | ||
| − | + | * [{{SERVER}}/library/index.php?/tags/226-glomerulonephritis PEIR Digital Library: Glomerulonephritis Images] | |
| + | * [http://library.med.utah.edu/WebPath/RENAHTML/RENALIDX.html#8 WebPath: Glomerulonephritis] | ||
== Related IPLab Cases == | == Related IPLab Cases == | ||
| − | + | * [[IPLab:Lab 1:Kidney Infarction|Lab 1: Kidney: Infarction (Coagulative Necrosis)]] | |
{{IPLab 6}} | {{IPLab 6}} | ||
[[Category: IPLab:Lab 6]] | [[Category: IPLab:Lab 6]] | ||
Latest revision as of 23:40, 8 July 2020
Contents
Clinical Summary[edit]
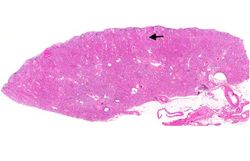
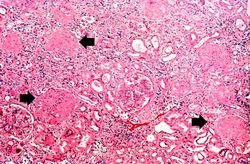
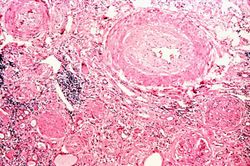
This 27-year-old male had end-stage renal disease requiring hemodialysis for 10 years. For the previous four years he had hypertension which slowly increased to about 180/120 mm Hg. Laboratory findings included a markedly elevated BUN and creatinine. He underwent bilateral nephrectomy and was placed on the transplant list.
On examination the kidneys were similar in appearance. Cortices were pale, diffusely granular with a few 1-2 mm cysts. On being sectioned, the cortex of each kidney was thin (4-5 mm) and pale. Renal medullae were pale yellow-tan in color and there was abundant peripelvic fat. The ureters, pelvis, calyces and hilar vessels showed no abnormalities.
Images[edit]
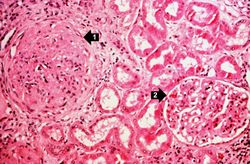
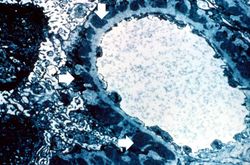
This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern.
Virtual Microscopy[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Assessment and Management of the Renal Transplant Patient
- eMedicine Medical Library: Poststreptococcal Glomerulonephritis
- Merck Manual: Nephritic Syndrome
- Merck Manual: Chronic Kidney Disease
- Merck Manual: Hemodialysis
- Merck Manual: Kidney Transplantation
Journal Articles[edit]
- Lan HY, Yang N, Nikolic-Paterson DJ, Yu XQ, Mu W, Isbel NM, Metz CN, Bucala R, Atkins RC. Expression of macrophage migration inhibitory factor in human glomerulonephritis. Kidney Int 2000 Feb;57(2):499-509.
Images[edit]
Related IPLab Cases[edit]
A normal alkaline phosphatase is 39 to 117 U/L.
These tests are measures of kidney function. High levels mean low function.
Oliguria is the occurrence of decreased urine output.
Hematuria is the presence of blood in the urine.