Difference between revisions of "IPLab:Lab 13:Meningococcemia"
Seung Park (talk | contribs) |
(→Clinical Summary) |
||
| (8 intermediate revisions by 2 users not shown) | |||
| Line 2: | Line 2: | ||
This 20-month-old black female was active and without complaint until 4 p.m. on the evening prior to her death, when according to her mother she acted as if she did not feel well. The mother reported that the child had felt warm at bedtime (8 p.m.) so she had given her some acetaminophen. At midnight, the child was given another dose of acetaminophen. The child slept with her mother that night who reported last hearing her daughter make a sound at approximately 7:30 a.m. The mother checked in on her daughter at 8:45 a.m. and found her to be unresponsive. The girl was dead when paramedics arrived. Her past medical history was unremarkable and there had been no recent illness among other family members. | This 20-month-old black female was active and without complaint until 4 p.m. on the evening prior to her death, when according to her mother she acted as if she did not feel well. The mother reported that the child had felt warm at bedtime (8 p.m.) so she had given her some acetaminophen. At midnight, the child was given another dose of acetaminophen. The child slept with her mother that night who reported last hearing her daughter make a sound at approximately 7:30 a.m. The mother checked in on her daughter at 8:45 a.m. and found her to be unresponsive. The girl was dead when paramedics arrived. Her past medical history was unremarkable and there had been no recent illness among other family members. | ||
| − | + | At autopsy external examination revealed multiple purpuric and ecchymotic cutaneous lesions, most notable in the inguinal areas. Microscopic examination of these skin lesions revealed thrombosis and rupture of small dermal vessels. There were scattered visceral petechial hemorrhages and both adrenal glands were grossly hemorrhagic. There was no gross or microscopic evidence of meningitis. However, a Gram stain of cerebrospinal fluid showed Gram-negative diplococci. Cultures were positive for Neisseria meningitides. | |
| − | |||
== Images == | == Images == | ||
| Line 16: | Line 15: | ||
File:IPLab13Meningococcemia8.jpg|This is a higher-power photomicrograph of a smear of cerebrospinal fluid taken at autopsy. Note the Gram-negative cocci in this smear, indicative of N. meningitidis. | File:IPLab13Meningococcemia8.jpg|This is a higher-power photomicrograph of a smear of cerebrospinal fluid taken at autopsy. Note the Gram-negative cocci in this smear, indicative of N. meningitidis. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="What is the Waterhouse-Friderichsen syndrome?">This is a syndrome consisting of the sudden onset of rapidly progressing illness with shock, cyanosis, hemorrhagic skin lesions, bilateral adrenal cortical hemorrhage, and usually death within 24 hours. It is the result of fulminant bacterial sepsis, often due to Neisseria meningitides, although many other organisms can be involved. N. meningitides releases a toxin that damages endothelial cells in small vessels all over the body. In the adrenal, this vascular damage and subsequent thrombosis leads to hemorrhagic necrosis.</spoiler> | ||
| + | * <spoiler text="What is the source of Neisseria meningitides?">Man is the only host. The organism lives in the nasopharynges of apparently unaffected individuals.</spoiler> | ||
| + | * <spoiler text="What is the favorite site of growth of Neisseria meningitides during clinical illness?">Cerebrospinal fluid is the favorite site of growth for the bacteria and meningitis is the most common illness. Other sites include heart valves, pericardium, joints, and the lungs.</spoiler> | ||
| + | |||
| + | == Additional Resources == | ||
| + | === Reference === | ||
| + | * [http://emedicine.medscape.com/article/221473-overview eMedicine Medical Library: Meningococcemia] | ||
| + | * [http://www.merckmanuals.com/professional/neurologic_disorders/meningitis/acute_bacterial_meningitis.html Merck Manual: Acute Bacterial Meningitis] | ||
| + | |||
| + | === Journal Articles === | ||
| + | * Leclerc F, Leteurtre S, Cremer R, Fourier C, Sadik A. [http://www.ncbi.nlm.nih.gov/pubmed/11007200 Do new strategies in meningococcemia produce better outcomes?] ''Crit Care Med'' 2000 Sep;28(9 Suppl):S60-3. | ||
| + | |||
| + | === Images === | ||
| + | * [{{SERVER}}/library/index.php?/tags/2175-meningococcus PEIR Digital Library: Meningococcemia Images] | ||
| + | * [{{SERVER}}/library/index.php?/tags/2176-adrenal_hemorrhage PEIR Digital Library: Adrenal Hemorrhage Images] | ||
{{IPLab 13}} | {{IPLab 13}} | ||
[[Category: IPLab:Lab 13]] | [[Category: IPLab:Lab 13]] | ||
Latest revision as of 21:37, 9 July 2020
Contents
Clinical Summary[edit]
This 20-month-old black female was active and without complaint until 4 p.m. on the evening prior to her death, when according to her mother she acted as if she did not feel well. The mother reported that the child had felt warm at bedtime (8 p.m.) so she had given her some acetaminophen. At midnight, the child was given another dose of acetaminophen. The child slept with her mother that night who reported last hearing her daughter make a sound at approximately 7:30 a.m. The mother checked in on her daughter at 8:45 a.m. and found her to be unresponsive. The girl was dead when paramedics arrived. Her past medical history was unremarkable and there had been no recent illness among other family members.
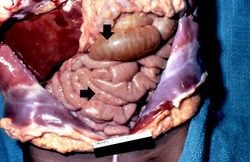
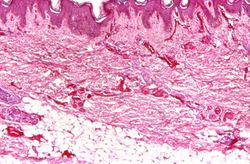
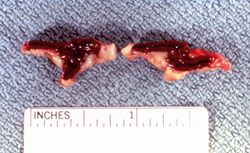
At autopsy external examination revealed multiple purpuric and ecchymotic cutaneous lesions, most notable in the inguinal areas. Microscopic examination of these skin lesions revealed thrombosis and rupture of small dermal vessels. There were scattered visceral petechial hemorrhages and both adrenal glands were grossly hemorrhagic. There was no gross or microscopic evidence of meningitis. However, a Gram stain of cerebrospinal fluid showed Gram-negative diplococci. Cultures were positive for Neisseria meningitides.
Images[edit]
This photomicrograph of the skin shows thrombi and fibrin clots in small vessels in the dermis. This is indicative of the endothelial damage caused by the Neisseria meningitidis endotoxin. This endotoxin-induced damage to the endothelium of small blood vessels throughout the body results in widespread petechiae and purpura.
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
Journal Articles[edit]
- Leclerc F, Leteurtre S, Cremer R, Fourier C, Sadik A. Do new strategies in meningococcemia produce better outcomes? Crit Care Med 2000 Sep;28(9 Suppl):S60-3.
Images[edit]
| |||||
Cyanosis is a bluish discoloration of the skin and mucous membranes resulting from increased concentrations of reduced hemoglobin in the blood. Cyanosis occurs when the blood oxygen saturation falls below 85%.