Difference between revisions of "IPLab:Lab 6:Chronic Rejection"
Seung Park (talk | contribs) (→Images) |
Seung Park (talk | contribs) |
||
| Line 20: | Line 20: | ||
File:IPLab6ChronicRejection12.jpg|Photomicrograph from another region of previous image. Note the cellular infiltrate around a small blood vessel (right) and neutrophils within renal tubules (arrow). | File:IPLab6ChronicRejection12.jpg|Photomicrograph from another region of previous image. Note the cellular infiltrate around a small blood vessel (right) and neutrophils within renal tubules (arrow). | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Virtual Microscopy == | ||
| + | <peir-vm>IPLab6ChronicRejection</peir-vm> | ||
== Study Questions == | == Study Questions == | ||
Revision as of 16:20, 3 January 2014
Contents
Clinical Summary[edit]
This 39-year-old male had malignant hypertension with malignant nephrosclerosis, progressing to chronic renal failure. He underwent a bilateral nephrectomy for control of his hypertension and received a cadaveric renal transplant. He did well, although he developed diabetes mellitus and had persistent, but less severe controllable hypertension. Two years following transplantation he was admitted to the hospital for control of his hypertension and evaluation of his chronic rejection. Initial blood pressure while in the hospital was in the range of 160/110 to 160/100 mm Hg. He was placed on a more intensive hypertension regimen, and he gradually became normotensive. He received one hemodialysis treatment prior to discharge. At the time of discharge, his blood pressure was 100 to 110 over 60 to 70 and he was doing well on dialysis. His BUN was 113 mg/dL and creatinine 5.2 mg/dL, and he had a hematocrit (PCV) of 27%. The patient was again admitted one month later for evaluation of azotemia and for control of his hypertension. It was felt that his chronic rejection was end-stage and that he would have to be dialyzed periodically. He was put on a renal failure diet, and over the period of his hospitalization, his BUN and creatinine finally stabilized at high levels. He tolerated dialysis well, and a transplant nephrectomy was done at 2 1/2 years post transplant. At the time of discharge, the patient's BUN was 78 mg/dL, creatinine 3.6 mg/dL, WBC 5000 cells/mm³, and the PCV was 26%.
Surgical Pathology Findings[edit]
The kidney weighed 215 grams and was covered by a thick capsule, which was partially adherent to the cortex, but could be stripped from the kidney with slight difficulty. The calyces and pelvis of the kidney appeared normal. The vessels were not prominent. The renal arteries and vein appeared normal.
Images[edit]
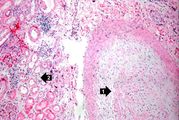
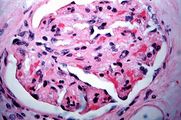
This is a higher-power photomicrograph of kidney containing a section of blood vessel that demonstrates a marked neointimal proliferative response (1). In this case the lumen of the artery is obliterated. Also note the cellular infiltrate in the interstitium of the kidney (2) and the paucity of tubules.
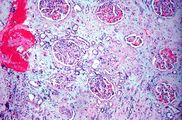
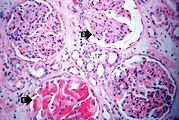
This is a photomicrograph of kidney with a focal area of hemorrhage around a small blood vessel (left) and congestion of the glomeruli. Note that there is a marked loss of renal tubules throughout this section with replacement by fibrous connective tissue. Also note the cellularity of the glomeruli.
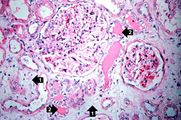
This is another area of renal cortex similar to the previous image. Note the fibrosis (1) and loss of renal tubules throughout this section. Also note the focus of inflammatory cells (2) indicating that despite the chromic nature of this lesion, there is still ongoing active rejection and renal damage.
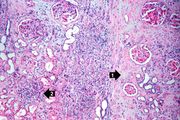
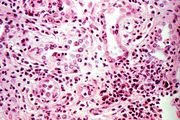
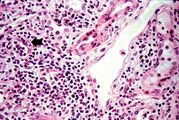
This is a high-power photomicrograph of a kidney from another case of chronic transplant rejection. In this case there is extensive damage to the kidney due to the chronic rejection (loss of tubules and glomerular lesions). In addition, this kidney was removed during an episode of acute rejection. The marked cellular infiltrate indicates acute rejection in a case of chronic transplant rejection.
Virtual Microscopy[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Assessment and Management of the Renal Transplant Patient
- eMedicine Medical Library: Renal Transplantation
- eMedicine Medical Library: Malignant Hypertension
- Merck Manual: Hypertensive Emergencies
- Merck Manual: Chronic Kidney Disease
- Merck Manual: Hemodialysis
- Merck Manual: Kidney Transplantation
Journal Articles[edit]
- Matas AJ. Impact of acute rejection on development of chronic rejection in pediatric renal transplant recipients. Pediatr Transplant 2000 May;4(2):92-9.
Images[edit]
Related IPLab Cases[edit]
- Lab 1: Kidney: Infarction (Coagulative Necrosis)
- Lab 6: Kidney: Acute Transplant Rejection
- Lab 10: Kidney: Candidiasis
Hypertension which has caused end-organ damage is termed malignant. Without proper treatment, these patients will usually die in less than 2 years. Blood pressures in patients with malignant hypertension are frequently 160/110 mm Hg or greater.
Renal failure is the severe reduction of renal function and often leads to reduced urinary output.
A normal BUN for this patient would be 10 to 20 mg/dL.
The normal creatinine level is 0.7 to 1.3 mg/dL.
A normal hematocrit for a male is 39 to 49%.
Azotemia is a condition of having excess nitrogen in the blood--a good indicator of reduced kidney function.
These tests are measures of kidney function. High levels mean low function.
A normal white blood cell count is 4000-11,000 cells/mm³.
A normal partial thromboplastin time is 28 to 37 seconds.
A normal kidney weighs 157 grams (range: 115 to 220 grams).
An infiltrate is an accumulation of cells in the lung parenchyma--this is a sign of pneumonia.