Difference between revisions of "IPLab:Lab 13:Biliary Atresia"
Seung Park (talk | contribs) |
|||
| Line 11: | Line 11: | ||
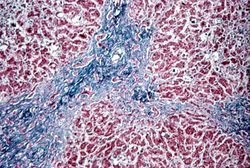
File:IPLab13BiliaryAtresia5.jpg|This is a medium-power photomicrograph of liver section stained with a trichrome stain to demonstrate the portal fibrosis. The fibrous connective tissue (collagen) stains blue. | File:IPLab13BiliaryAtresia5.jpg|This is a medium-power photomicrograph of liver section stained with a trichrome stain to demonstrate the portal fibrosis. The fibrous connective tissue (collagen) stains blue. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="How common is biliary atresia?">Biliary atresia occurs in approximately 1 out of 10,000 live births.</spoiler> | ||
| + | * <spoiler text="What are the usual presenting signs?">Neonatal cholestasis. | ||
| + | |||
| + | A major cause of neonatal cholestasis (1/3 of cases) is extrahepatic biliary atresia (EHBA).</spoiler> | ||
| + | * <spoiler text="What is the pathogenesis of biliary atresia?">In most cases of EHBA the infants are born with a normal biliary tree. However, within the first few weeks of life the bile ducts are destroyed. | ||
| + | |||
| + | There are numerous theories as to the etiology of the inflammatory process that destroys the bile ducts in these newborns. These include: | ||
| + | # viral infections (reovirus 3, cytomegalovirus, and rubella virus); | ||
| + | # genetic inheritance (EHBA has been reported in twins and there are descriptions of EHBA occurring in families with anomalies of the intrahepatic biliary tree); and | ||
| + | # abnormal embryologic development--15 to 20% of EHBA patients have extrahepatic anomalies such as polysplenism, cardiovascular defects, and bowel atresias.</spoiler> | ||
| + | * <spoiler text="What is the standard treatment for extra-hepatic biliary atresia?">Liver transplantation.</spoiler> | ||
{{IPLab 13}} | {{IPLab 13}} | ||
[[Category: IPLab:Lab 13]] | [[Category: IPLab:Lab 13]] | ||
Revision as of 16:13, 21 August 2013
Clinical Summary[edit]
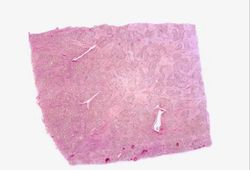
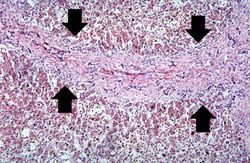
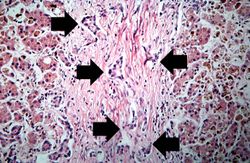
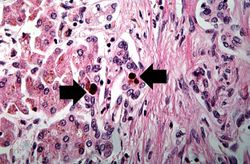
This eight-month-old female developed jaundice at one week of age. As the jaundice deepened, the child's bilirubin level was found to be over 30 mg/dL and the patient experienced a few convulsive episodes. A liver biopsy produced a diagnosis of extrahepatic bile duct obstruction. A subsequent exploratory laparotomy showed an absence of extrahepatic bile duct structures--including the gallbladder--and an intraoperative cholangiogram failed to show any large biliary channel. A jejunohepatostomy in the portal area was performed in the hope of establishing bile drainage and the patient was placed on the waiting list for a liver transplant. However, the patient progressively deteriorated, developed infections, and after a long turbulent course, died of pneumonia.
Images[edit]
Study Questions[edit]
| |||||
Jaundice (or icterus) is a state of hyperbilirubinemia (increased bilirubin in the blood) in which bile pigment is deposited in the skin, mucous membranes, and scleras. This deposition of bile pigment results in a yellow appearance.
A normal bilirubin level for a child this age would be <2 mg/dL.
Transhepatic cholangiography involves the injection of a radiopaque dye into the intrahepatic ducts of patients with obstructive jaundice. Radiographs are then taken to determine whether a route exists for the dye to leave the liver.
A jejunohepatostomy is a procedure in which an attempt is made to bypass the biliary tree by having bile drain into the jejunum. Risks of this procedure include the development of bacterial infections of the intrahepatic biliary tree.
Liver transplantation (along with the donor's bile ducts) is the most successful treatment for these patients.
In alcoholics, aspiration pneumonia is common--bacteria enter the lung via aspiration of gastric contents.