Difference between revisions of "IPLab:Lab 13:Myelomeningocele"
Seung Park (talk | contribs) |
|||
| Line 17: | Line 17: | ||
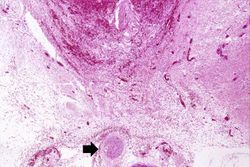
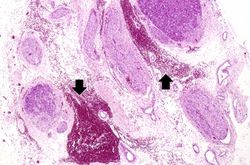
File:IPLab13Myelomeningocele7.jpg|This high-power photomicrograph of the spinal cord within the vertebral column shows the hemorrhage (arrows) in this region. | File:IPLab13Myelomeningocele7.jpg|This high-power photomicrograph of the spinal cord within the vertebral column shows the hemorrhage (arrows) in this region. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="What are the various types of neural tube defects?">Neural tube defects (NTD) are abnormalities of both neural tissue and overlying bone and/or soft tissues which result in failure to close of a portion of the neural tube or reopening of a region that had previously been closed. The most common forms of NTD in newborns involve the caudal portions of the spinal cord. | ||
| + | |||
| + | NTDs may include: | ||
| + | * Anencephaly - malformation of the anterior neural tube leading to failure of the brain and calvarium to develop | ||
| + | * Encephalocele - diverticulum of malformed brain tissue extending through a hole in the cranium. | ||
| + | * Spinal dysraphism or spina bifida - asymptomatic bony defect (spina bifida occulta) or a severe malformation with a flattened, disorganized segment of spinal cord, associated with an overlying meningeal out-pouching. | ||
| + | * Meningocele - defect in the spinal column with meningeal tissue extending through it. | ||
| + | * Myelomeningocele - defect in the spinal column with meningeal and spinal cord tissue extending through it.</spoiler> | ||
| + | * <spoiler text="What is the etiology of neural tube defects?">The etiology of NTDs is generally unknown, though most NTDs appear to be due to multifactorial inheritance and environmental factors. | ||
| + | |||
| + | The frequency of NTDs varies widely among ethnic groups and there is a recurrence rate for NTDs in subsequent pregnancies of approximately 4 to 5%. | ||
| + | |||
| + | Recent evidence has shown that folate deficiency during the first few weeks of gestation increases the risk of NTDs. Other risk factors include diabetes mellitus, hyperthermia, alcohol ingestion and exposure to other toxic substances.</spoiler> | ||
| + | * <spoiler text="What kinds of clinical problems can be seen in patients with myelomeningoceles?">Clinical problems can result from damage to the spinal cord due to the myelomeningocele or due to secondary infection. | ||
| + | |||
| + | Clinical deficits usually occur in motor and sensory function in the lower extremities as well as disturbances of bowel and bladder control.</spoiler> | ||
{{IPLab 13}} | {{IPLab 13}} | ||
[[Category: IPLab:Lab 13]] | [[Category: IPLab:Lab 13]] | ||
Revision as of 16:11, 21 August 2013
Clinical Summary[edit]
This male fetus of a 21-year-old Rh-positive mother (Gravida 2 Para 1011) was the product of an induced delivery at 21 weeks gestation. At 19 weeks gestation, routine prenatal examination had revealed a maternal serum alpha-fetoprotein (AFP) level that was 4.2 times the mean for a mother at this point in gestation. A targeted ultrasound was ordered--which revealed a lumbosacral neural tube defect--and an amniocentesis was performed. Amniotic fluid showed an AFP level that was 5.3 times the calculated median value and cytogenetic analysis demonstrated a normal male (46XY) chromosome pattern. The parents requested termination of the pregnancy and a 465-gram male nondysmorphic stillborn fetus was delivered vaginally.
Autopsy Findings[edit]
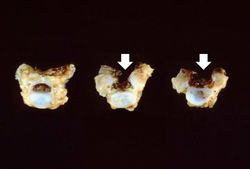
There was a myelomeningocele in the lumbar region that measured 1.6 cm in width and 3.7 cm in length.
Images[edit]
Study Questions[edit]
| |||||
Rh-positive infants of Rh-negative mothers are at particular risk of developing erythroblastosis fetalis (hemolytic disease of newborns) unless preventive treatments are administered. Successful screening for maternal Rh-negativity and subsequent preventive treatment has greatly reduced the incidence of Rh-induced erythroblastosis fetalis. However, ABO incompatibility between the mother and fetus can also cause erythroblastosis fetalis. Thus, the fact that this mother was Rh-positive does not protect the fetus from developing ABO-induced incompatibility if the mother and fetus have different ABO blood types.
Gravida and para are forms of Latin words which are used in clinical notation. Gravida indicates the number of pregnancies which a woman has had (including a current pregnancy). Thus a pregnant woman with two previous pregnancies (regardless of the outcomes of the pregnancies) would be considered Gravida 3 (abbreviated G3). Para indicates the outcomes of a woman's pregnancies. It is represented by four numbers. First number: term births. Second number: preterm births. Third number: abortions. Fourth number: living children. A woman who is currently pregnant and who has had two previous pregnancies--one child being born preterm and the other term, both now living--would be listed as G3 P1102. A current pregnancy is not included because the outcome is not yet known.
The normal gestation period is 38 to 42 weeks.
Alpha-fetoprotein (AFP) is a serum glycoprotein produced during pregnancy by the yolk sac, fetal GI tract, and fetal liver. Elevated serum AFP levels in a pregnant woman can be an indication of a fetal neural tube defect (or something as common as multiple pregnancy). Open fetal neural tube defects allow alpha-fetoprotein to leak into the amniotic fluid, from which it crosses the placenta and enters the maternal bloodstream. Elevated maternal AFP is an indication for amniocentesis (of which an AFP level of amniotic fluid is routine) and an ultrasound. The combination of these two tests are very reliable in detecting neural tube defects.
Alpha-fetoprotein (AFP) is a serum glycoprotein produced during pregnancy by the yolk sac, fetal GI tract, and fetal liver. Elevated serum AFP levels in a pregnant woman can be an indication of a fetal neural tube defect (or something as common as multiple pregnancy). Decreased serum levels are indicative of trisomy 21.
A maternal serum AFP level is considered elevated if it is greater than 2.5 times the mean.
The neural plate is a part of the dorsal ectoderm from which the central nervous system develops. During fetal development, this plate folds longitudinally to form the neural tube which is protected by the eventual development of surrounding mesoderm into the skull, vertebral column, and skin. A neural tube defect occurs when this surrounding mesoderm does not properly enclose around the neural tube.
Amniocentesis is a procedure in which a needle is inserted transabdominally through the uterus, into the amniotic sac, and amniotic fluid is withdrawn.
A normal male fetus at this age of development should weigh 360 to 492 grams.
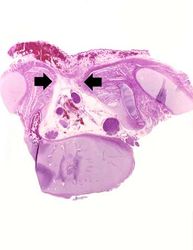
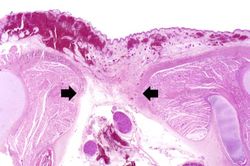
A myelomeningocele is the herniation of the spinal cord--within the meninges--through a defect in the vertebral canal.