Difference between revisions of "IPLab:Lab 5:α1 Antitrypsin Deficiency"
Seung Park (talk | contribs) |
Seung Park (talk | contribs) |
||
| Line 1: | Line 1: | ||
== Clinical Summary == | == Clinical Summary == | ||
| − | This 68-year-old white female was afflicted with severe emphysema due to | + | This 68-year-old white female was afflicted with severe emphysema due to α1-antitrypsin deficiency. She had a 10 pack-year history of cigarette smoking but she had quit smoking 30 years ago. She elected to undergo lung volume reduction surgery to reduce complications of her emphysema. Post-operatively, she was ventilator dependent and her liver function declined. Further studies revealed hepatic cirrhosis. Her pulmonary function continued to decline and she died 26 days after her initial surgery. |
== Autopsy Findings == | == Autopsy Findings == | ||
| Line 18: | Line 18: | ||
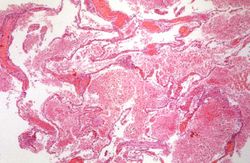
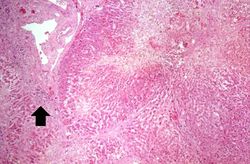
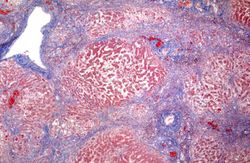
File:IPLab5Antitrypsin10.jpg|This is a low-power photomicrograph of a trichrome-stained section of liver. There is bridging fibrosis (blue material) between portal regions. | File:IPLab5Antitrypsin10.jpg|This is a low-power photomicrograph of a trichrome-stained section of liver. There is bridging fibrosis (blue material) between portal regions. | ||
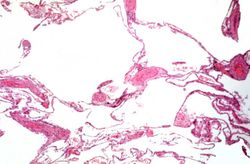
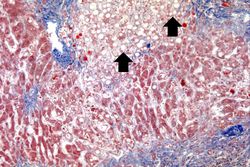
File:IPLab5Antitrypsin11.jpg|This is a higher-power photomicrograph of a trichrome-stained section of liver. This section demonstrates the fibrosis (blue material) and the fatty change (arrows). | File:IPLab5Antitrypsin11.jpg|This is a higher-power photomicrograph of a trichrome-stained section of liver. This section demonstrates the fibrosis (blue material) and the fatty change (arrows). | ||
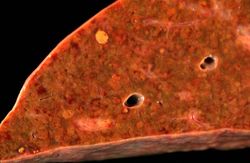
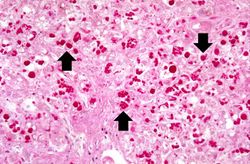
| − | File:IPLab5Antitrypsin12.jpg|This is a high-power photomicrograph of liver stained with periodic-acid Schiff's (PAS) stain. This demonstrates the PAS-positive granules of defective | + | File:IPLab5Antitrypsin12.jpg|This is a high-power photomicrograph of liver stained with periodic-acid Schiff's (PAS) stain. This demonstrates the PAS-positive granules of defective α1-antitrypsin that accumulate in the Golgi of hepatocytes (arrows). |
</gallery> | </gallery> | ||
== Study Questions == | == Study Questions == | ||
| − | * <spoiler text="What is the genetic defect and pattern of inheritance in | + | * <spoiler text="What is the genetic defect and pattern of inheritance in α1-antitrypsin deficiency?">α1-antitrypsin deficiency is an autosomal recessive disorder caused by mutations in the protease inhibitor locus of chromosome 14. In the mutations that lead to a deficiency of the enzyme, the protein is transcribed but there is abnormal folding of the protein, thus it cannot be processed by the endoplasmic reticulum of hepatocytes. The protein, therefore, accumulates in the endoplasmic reticulum forming PAS-positive granules.</spoiler> |
| − | * <spoiler text="What is the pathogenesis of emphysema in patients with | + | * <spoiler text="What is the pathogenesis of emphysema in patients with α1-antitrypsin deficiency?">α1-antitrypsin is the major antiprotease and is responsible for inhibiting neutrophil elastase that can cause destruction of the alveolar wall. With α1-antitrypsin deficiency, neutrophil elastase goes unchecked and tissue damage ensues.</spoiler> |
| − | * <spoiler text="What role does smoking play in the development of emphysema in patients with | + | * <spoiler text="What role does smoking play in the development of emphysema in patients with α1-antitrypsin deficiency?">Smoking increases the numbers of neutrophils in the lung and accentuates the release of elastase from these neutrophils. With a deficiency of α1-antitrypsin there is marked tissue damage.</spoiler> |
| − | * <spoiler text="Is hepatic cirrhosis common in patients with | + | * <spoiler text="Is hepatic cirrhosis common in patients with α1-antitrypsin deficiency and what is the pathogenesis of the cirrhosis?">The abnormal α1-antitrypsin protein accumulates in hepatocytes of all patients with this abnormality but only 8 to 20% develop cirrhosis. The exact mechanism for hepatic cirrhosis in patients with α1-antitrypsin deficiency is not well understood.</spoiler> |
{{IPLab 5}} | {{IPLab 5}} | ||
[[Category: IPLab:Lab 5]] | [[Category: IPLab:Lab 5]] | ||
Revision as of 17:16, 21 August 2013
Clinical Summary[edit]
This 68-year-old white female was afflicted with severe emphysema due to α1-antitrypsin deficiency. She had a 10 pack-year history of cigarette smoking but she had quit smoking 30 years ago. She elected to undergo lung volume reduction surgery to reduce complications of her emphysema. Post-operatively, she was ventilator dependent and her liver function declined. Further studies revealed hepatic cirrhosis. Her pulmonary function continued to decline and she died 26 days after her initial surgery.
Autopsy Findings[edit]
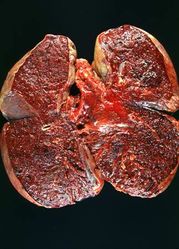
There were severe emphysematous changes in all lung lobes and there was massive hemorrhage throughout the lungs (combined lung weight: 3510 grams). The liver weighed 860 grams and there was micronodular cirrhosis.
Images[edit]
This is a gross photograph of the lungs from this case. The rough friable material on the surface of the lung (arrows) is fibrinous exudate and fibrous tissue. This reaction on the surface of the lung is due to the recent surgery. The emphysematous changes are not easily appreciated in this photograph.
Study Questions[edit]
| |||||
Pulmonary emphysema is a condition in which the air spaces distal to the terminal bronchioles are permanently increased in size due to either destruction of the wall or alveolar dilatation.
A pack-year denotes smoking one pack of cigarettes per day for one year.
Cirrhosis is a liver disease characterized by necrosis, fibrosis, loss of normal liver architecture, and hyperplastic nodules.
A normal partial thromboplastin time is 28 to 37 seconds.
Friable material is easily crumbled.
Consolidation is the filling of lung air spaces with exudate--this is a sign of pneumonia.