IPLab:Lab 2:Hypertrophy
Contents
Clinical Summary[edit]
This 68-year-old man initially sought medical advice five years prior to his death. His symptoms at that time were exercise intolerance and occasional peripheral edema. He gave a history of a "heart murmur" that was diagnosed 25 years ago during an employment physical. No follow up care had been given for this murmur.
The patient's terminal admission was for signs of severe heart failure -- the patient had marked peripheral edema and shortness of breath and chest x-ray revealed significant cardiac enlargement and pulmonary edema with bilateral pleural effusions. He sustained a cardiac arrest shortly after admission and could not be resuscitated.
Autopsy Findings[edit]
Autopsy disclosed a markedly enlarged heart weighing 650 grams and having dilated chambers. The aortic valve was calcified and showed evidence of stenosis and insufficiency. The coronary arteries were narrowed 60 to 70% by atherosclerosis. No acute coronary occlusions were found and there was no evidence of myocardial infarction.
Images[edit]
This is a gross photograph of a cross section of a normal human heart taken at autopsy (right) and the heart from this case, which demonstrates concentric hypertrophy of the left ventricular wall. Note the marked thickening of the left ventricular wall. There is also moderate thickening of the right ventricular wall.
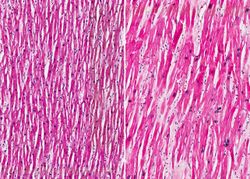
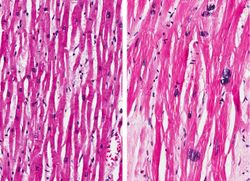
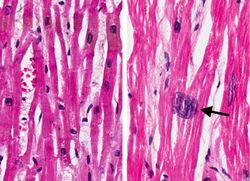
Normal myocardium (left) is compared to hypertrophied myocardium (right). This high power view demonstrates the large dark nuclei (arrow) found in hypertrophied cardiac muscle cells. Polyploidy is a common feature in cardiac hypertrophy. Also note the increased size (thickness) of the individual cardiac muscle cell on the right compared to normal cardiac myocytes (left).
This autopsy specimen was taken from another patient who had cardiac hypertrophy and congestive heart failure that resulted in dilation of the cardiac chambers. This heart was markedly enlarged (700 grams) but the congestive failure leads to dilation of the chambers and thinning of the wall. Note the marked dilation of both the left (1) and right (2) ventricular chambers.
This gross photograph shows an example of normal physiologic hypertrophy. The organs shown are an open uterus (1), cervix (2) and vagina (3), both ovaries (4) and both kidneys (5) from a woman who died shortly after normal delivery from causes unrelated to childbirth. Note the marked thickening of the uterine wall due to smooth muscle cell hypertrophy.
Virtual Microscopy[edit]
Myocardial Hypertrophy[edit]
Normal Heart[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Pediatric Hypertrophic Cardiomyopathy
- eMedicine Medical Library: Heart Failure
- Merck Manual: Hypertrophic Cardiomyopathy
- Merck Manual: Heart Failure
Journal Articles[edit]
- Amann K, Rychlík I, Miltenberger-Milteny G, Ritz E. Left ventricular hypertrophy in renal failure. Kidney Int Suppl 1998 Dec;68:S78-85.
- Khan IA, Ajatta FO, Ansari AW. Persistent ST segment elevation: a new ECG finding in hypertrophic cardiomyopathy. Am J Emerg Med 1999 May;17(3):296-9.
Images[edit]
- PEIR Digital Library: Cardiomyopathy Images
- PEIR Digital Library: Cardiac Hypertrophy Images
- WebPath: Cardiomyopathies
Related IPLab Cases[edit]
| |||||
Exercise intolerance is the development of shortness of breath upon exertion.
Peripheral edema refers to the accumulation of fluid in the intercellular tissue spaces of the legs and ankles.
Marked peripheral edema is usually a manifestation of heart failure -- especially of the right ventricle.
Shortness of breath is a common clinical manifestation of heart failure.
Pulmonary edema refers to the accumulation of abnormal amounts of fluid in the extravascular spaces of the lungs. There are many causes for pulmonary edema. However, it is common clinical manifestation of left ventricular heart failure. Pressures rise in the left atrium and ventricle to compensate for the failure and this causes increased pressure in the pulmonary vasculature. Incrased pulmonary capillary pressure relative to the plasma oncotic pressure cause fluid to leave the vessels and enter the interstitial spaces of the lung.
Pleural effusion is the presence of fluid in the pleural space. Increased hydrostatic pressure in the pulmonary vasculature, as seen in heart failure, is one cause of pleural effusion.
Cardiac arrest is the sudden standstill of cardiac function.
A normal heart weighs 300 grams (range: 270 to 360 grams).
Aortic stenosis (calcification of the aortic valve) is the most common valve abnormality. Calcification of the valve leads to a reduced valve area. Increased pressure is thus needed from the left ventricle to pump blood into the aorta. Over time, the pressure-overloaded ventricle hypertrophies concentrically (increased ratio of wall thickness to cavity radius) in an attempt to reduce wall tension (review the Law of Laplace). Eventually, the left ventricle's contractile capacity is overwhelmed by the stiffness of the ventricle (due to hypertrophy) and pressure begins to increase through the left atrium and into the pulmonary vasculature. Increased pulmonary artery pressures then lead to right ventricular failure.
Aortic insufficiency refers to the inability of the aortic valve to close properly, thus allowing regurgitation of blood into the left ventricle during diastole -- i.e., volume overload. Disease of the aortic valve leaflets is a common cause of insufficiency.
Myocardial infarction is necrosis of myocardial tissue which occurs as a result of a deprivation of blood supply, and thus oxygen, to the heart tissue. Blockage of blood supply to the myocardium is caused by occlusion of a coronary artery.
Concentric hypertrophy is seen in pressure-overloaded hearts.
A normal heart weighs 300 grams (range: 270 to 360 grams).