Difference between revisions of "IPLab:Lab 12:Alcoholic Cirrhosis"
(→Clinical Summary) |
|||
| (9 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
== Clinical Summary == | == Clinical Summary == | ||
| + | This 56-year-old white male came to the emergency room because of weakness, lack of appetite, shortness of breath, abdominal distention, and an altered mental status. He was a known to have alcohol use disorder and he drank approximately one pint of whiskey per day. Physical examination revealed a protuberant abdomen, bilateral gynecomastia, and spider angiomata on his chest. Liver enzymes were elevated, albumin was low and he was anemic. | ||
| − | + | The patient was given thiamine, folate, multivitamins, and vitamin K and an intravenous line was placed to infuse 5% dextrose. An esophagogastroduodenoscopy (EGD) demonstrated large esophageal varices. Two days after admission the patient developed a massive hematemesis due to rupture of an esophageal varices and despite successful sclerotherapy and supportive transfusions, the patient died the next day. | |
== Images == | == Images == | ||
| Line 20: | Line 21: | ||
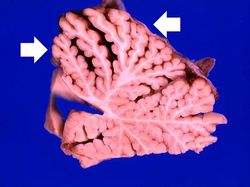
File:IPLab12Alcoholic14.jpg|This is another photograph of the cerebellum from this patient demonstrating the marked thinning of the anterior portion of the cerebellum (arrows). This pattern of cerebellar damage is consistent with Wernicke's encephalopathy. | File:IPLab12Alcoholic14.jpg|This is another photograph of the cerebellum from this patient demonstrating the marked thinning of the anterior portion of the cerebellum (arrows). This pattern of cerebellar damage is consistent with Wernicke's encephalopathy. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="How does alcohol cause liver damage?">Initial changes include hepatocellular steatosis. This is caused by altered metabolism with high levels of NADH from lactate dehydrogenase resulting in increased lipid biosynthesis. Mobilization of lipids from peripheral fat stores and decreased lipid acceptor protein synthesis leads to insufficient lipoprotein production. | ||
| + | |||
| + | Alcohol induces free radical production as it is broken down by the microsomal ethanol oxidizing system. Alcohol also impairs microtubular and mitochondrial function and membrane fluidity. | ||
| + | |||
| + | Acetaldehyde, the major ethanol metabolite, can cause lipid peroxidation and acetaldehyde-protein complexes that further inhibit the microtubular system. | ||
| + | |||
| + | Finally, alcohol also induces an immunologic reaction in the liver. This immune-mediated liver damage is thought to result from the expression of neoantigens on hepatocytes possibly due to alcohol-induced alterations in membranes or acetaldehyde binding to proteins leading to neoantigen formation.</spoiler> | ||
| + | * <spoiler text="Why did this patient have a prolonged prothrombin time?">Since most of the clotting factors are produced by the liver, chronic liver damage with loss of liver parenchyma will lead to a reduction in clotting factors. In addition, this patient had bleeding esophageal varices and ascites which could both use up or sequester clotting factors, respectively.</spoiler> | ||
| + | * <spoiler text="What causes esophageal varices in a patient with hepatic cirrhosis?">Hepatic cirrhosis with extensive parenchymal damage and fibrosis results in an increased resistance to portal blood flow. The increased portal pressure leads to increased pressure in the coronary veins of the stomach. This results in increased pressure in the esophageal plexus in the terminal portion of the esophagus as the blood travels through this plexus to empty into the azygous vein. The increased pressure and increased flow of blood through this plexus of thin-walled veins leads to dilation and formation of varices. These varices can then rupture and lead to life-threatening hemorrhage as was seen in this case. | ||
| + | |||
| + | Increased portal pressure also leads to increased pressure in the inferior hemorrhoidal veins and can lead to the formation of anorectal varices.</spoiler> | ||
| + | * <spoiler text="What is the pathogenesis of Wernicke's encephalopathy?">Wernicke's encephalopathy is caused by thiamine (Vitamin B1) deficiency. Chronic alcoholics often have poor diets and alcohol inhibits intestinal absorption of thiamine. Thus, some chronic alcoholics can develop Wernicke's encephalopathy which consists of foci of symmetric discoloration, softening, and punctate hemorrhages in the paraventricular regions of the thalamus and hypothalamus, in the mamillary bodies, around the aqueduct in the midbrain, in the floor of the fourth ventricle and in the anterior cerebellum. There is demyelinization and loss of neuropil. Even after treatment with thiamine, there is significant memory deficit.</spoiler> | ||
| + | |||
| + | == Additional Resources == | ||
| + | === Reference === | ||
| + | * [http://emedicine.medscape.com/article/185856-overview eMedicine Medical Library: Cirrhosis] | ||
| + | * [http://emedicine.medscape.com/article/366426-overview eMedicine Medical Library: Cirrhosis Imaging] | ||
| + | * [http://www.merckmanuals.com/professional/hepatic_and_biliary_disorders/alcoholic_liver_disease/alcoholic_liver_disease.html Merck Manual: Alcoholic Liver Disease] | ||
| + | |||
| + | === Journal Articles === | ||
| + | * Fujimoto J. [http://www.ncbi.nlm.nih.gov/pubmed/10759218 Gene therapy for liver cirrhosis]. ''J Gastroenterol Hepatol'' 2000 Mar;15 Suppl:D33-6. | ||
| + | * Ge PS and Runyon BA [http://www.nejm.org/doi/pdf/10.1056/NEJMra1504367 Treatment of Patients with Cirrhosis]. ''NEJM'' 2016 Aug 25 375(8):767. | ||
| + | |||
| + | === Images === | ||
| + | * [{{SERVER}}/library/index.php?/tags/128-cirrhosis PEIR Digital Library: Cirrhosis Images] | ||
| + | * [http://library.med.utah.edu/WebPath/LIVEHTML/LIVERIDX.html WebPath: Hepatic Pathology] | ||
| + | |||
| + | == Related IPLab Cases == | ||
| + | * [[IPLab:Lab 2:Fatty Change and Cirrhosis|Lab 2: Liver: Fatty Change and Cirrhosis]] | ||
{{IPLab 12}} | {{IPLab 12}} | ||
[[Category: IPLab:Lab 12]] | [[Category: IPLab:Lab 12]] | ||
Latest revision as of 21:10, 9 July 2020
Contents
Clinical Summary[edit]
This 56-year-old white male came to the emergency room because of weakness, lack of appetite, shortness of breath, abdominal distention, and an altered mental status. He was a known to have alcohol use disorder and he drank approximately one pint of whiskey per day. Physical examination revealed a protuberant abdomen, bilateral gynecomastia, and spider angiomata on his chest. Liver enzymes were elevated, albumin was low and he was anemic.
The patient was given thiamine, folate, multivitamins, and vitamin K and an intravenous line was placed to infuse 5% dextrose. An esophagogastroduodenoscopy (EGD) demonstrated large esophageal varices. Two days after admission the patient developed a massive hematemesis due to rupture of an esophageal varices and despite successful sclerotherapy and supportive transfusions, the patient died the next day.
Images[edit]
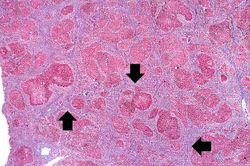
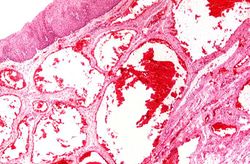
In this is medium-power photomicrograph of trichrome stained liver the bands of fibrous tissue are seen to form "bridges" between triad areas (arrows); this is called "bridging fibrosis." Also note the fibrous tissue (arrows) and how the hepatocytes are separated into nodules by this fibrous tissue.
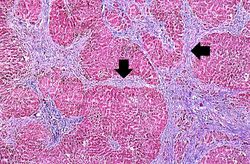
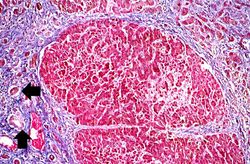
In this high-power photomicrograph of trichrome-stained liver, the bands of fibrous tissue surround the hepatocyte nodules. There is some degeneration and dropout of hepatocytes in this nodule. Also note the increased numbers of bile ducts in the triad area (arrows). Bile duct proliferation is a common feature in many hepatitides.
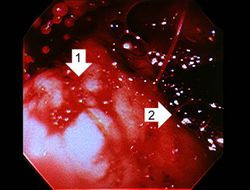
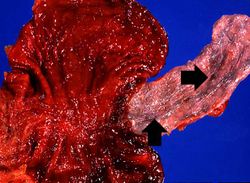
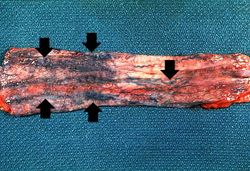
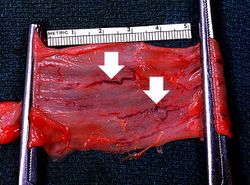
This photograph taken from still another patient at autopsy demonstrates the esophageal varices in the distal esophagus (arrows). The esophagus was clamped before removing the esophagus from the body in order to trap the blood in these distended varices. It is obvious how easily these thin-walled superficial varices could rupture and bleed.
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Cirrhosis
- eMedicine Medical Library: Cirrhosis Imaging
- Merck Manual: Alcoholic Liver Disease
Journal Articles[edit]
- Fujimoto J. Gene therapy for liver cirrhosis. J Gastroenterol Hepatol 2000 Mar;15 Suppl:D33-6.
- Ge PS and Runyon BA Treatment of Patients with Cirrhosis. NEJM 2016 Aug 25 375(8):767.
Images[edit]
Related IPLab Cases[edit]
| |||||
Shortness of breath is a common clinical manifestation of heart failure.
A focal network of small arteries and arterioles arranged in a radial pattern with a central red spot.
Hematemesis is the vomiting of blood.
Nodular hyperplasia of the prostate--characterized by large discrete prostatic nodules--is a common disorder in men over 50 years of age. The nodules cause the prostate to be enlarged and to have an increased weight. The human prostate is surrounded by a restrictive capsule. These nodules cause increased pressure within the capsule which leads to constriction of the urethra as it passes through the prostate. Urethral constriction leads to retention of urine.
Cirrhosis is a liver disease characterized by necrosis, fibrosis, loss of normal liver architecture, and hyperplastic nodules.