Difference between revisions of "IPLab:Lab 3:Fibrinous Pericarditis"
Seung Park (talk | contribs) |
Seung Park (talk | contribs) |
||
| Line 15: | Line 15: | ||
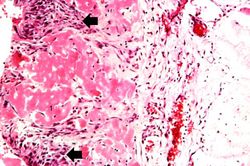
File:IPLab3FibrinousPericarditis5.jpg|This high-power photomicrograph demonstrates fibrin (red amorphous material) on the surface of the pericardium (1). Note the reactive mesothelial cells on the surface of the pericardium (arrows) and the inflammatory cells within the pericardial tissue. | File:IPLab3FibrinousPericarditis5.jpg|This high-power photomicrograph demonstrates fibrin (red amorphous material) on the surface of the pericardium (1). Note the reactive mesothelial cells on the surface of the pericardium (arrows) and the inflammatory cells within the pericardial tissue. | ||
</gallery> | </gallery> | ||
| + | |||
| + | Study Questions | ||
| + | * <spoiler text="What is the etiology of the fibrinous pericarditis that developed in this patient with renal failure?">Azotemia (an excess of nitrogen in the blood) is believed to be the cause of fibrinous pericarditis but the exact mechanism is unknown.</spoiler> | ||
| + | * <spoiler text="What are some other possible causes for pericarditis?">These include: | ||
| + | * infection -- viral, bacterial (especially TB), or fungal; | ||
| + | * rheumatic fever | ||
| + | * systemic lupus erythematosus; | ||
| + | * scleroderma; | ||
| + | * myocardial infarction; | ||
| + | * trauma; and | ||
| + | * neoplasia.</spoiler> | ||
| + | * <spoiler text="From where does the fibrin come that produces fibrinous pericarditis?">Fibrinogen leaks out of the blood vessels as part of the inflammatory reaction. It is then converted to fibrin. A fibrinous exudate develops when the vascular leaks are large enough or there is a procoagulant stimulus (e.g., pericarditis).</spoiler> | ||
| + | * <spoiler text="What are the possible outcomes of this condition (fibrinous pericarditis)?">* The inflammatory reaction can progress and lead to tamponade (rare). | ||
| + | * The inflammatory reaction could subside and the fibrin would be lysed via the fibrinolytic system (most likely outcome). | ||
| + | * The fibrin could become organized and result in a fibrous connective tissue scar which could restrict cardiac function.</spoiler> | ||
{{IPLab 3}} | {{IPLab 3}} | ||
[[Category:IPLab:Lab 3]] | [[Category:IPLab:Lab 3]] | ||
Revision as of 05:04, 19 August 2013
Clinical Summary[edit]
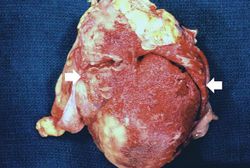
This patient is a 36-year-old white male with a history of long-standing renal disease who presents with end-stage kidney disease and a BUN of 112 mg/dL. During the present hospitalization he developed a pericardial friction rub and pericardial and pleural effusions. A semi-elective pericardiectomy was performed.
Findings[edit]
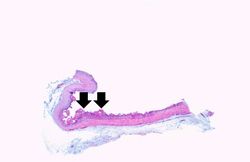
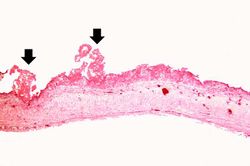
Submitted for examination was a rectangular segment of gray-tan tissue measuring 9.5 x 8.5 x 0.3 cm. The outer surface was fatty in appearance. The inner surface was rough and covered by a number of fine red papillary projections. The projections were composed of fine strands having the appearance of fibrin.
Images[edit]
Study Questions
A normal BUN for this patient would be 10 to 20 mg/dL.
A pericardial friction rub is the characteristic sign of pericarditis. It sounds like the rubbing together of two rough surfaces. The sound may vary over time and patient position.
Pleural effusion is the presence of fluid in the pleural space. Increased hydrostatic pressure in the pulmonary vasculature, as seen in heart failure, is one cause of pleural effusion.
A pericardiectomy is a surgical procedure in which the pericardial sac is opened, a piece is removed, and the sac is left open.
Pericarditis is inflammation of the pericardium - often with deposition of fibrin.
Myocardial infarction is necrosis of myocardial tissue which occurs as a result of a deprivation of blood supply, and thus oxygen, to the heart tissue. Blockage of blood supply to the myocardium is caused by occlusion of a coronary artery.