Difference between revisions of "IPLab:Lab 10:Mucormycosis"
(→Clinical Summary) |
|||
| (9 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
== Clinical Summary == | == Clinical Summary == | ||
| − | This 63-year-old white male was in his usual state of good health until eight weeks before his death when he developed sudden onset of shortness of breath. A thoracotomy was performed for plication of ruptured emphysematous blebs. Following improvement and discharge from the hospital he developed weakness, lethargy, and a left lower lobe lung infiltrate. The patient's condition soon deteriorated further, with almost every organ system having failed. The patient developed DIC and peripheral embolic phenomena, including gangrene of his extremities and face. A single antemortem blood culture grew Staphylococcus aureus. | + | This 63-year-old white male was in his usual state of good health until eight weeks before his death when he developed sudden onset of shortness of breath. A thoracotomy was performed for plication of ruptured emphysematous blebs. Following improvement and discharge from the hospital he developed weakness, lethargy, and a left lower lobe lung infiltrate. The patient's condition soon deteriorated further, with almost every organ system having failed. The patient developed DIC and peripheral embolic phenomena, including gangrene of his extremities and face. A single antemortem blood culture grew Staphylococcus aureus. |
| − | + | Autopsy revealed severe emphysema, severe widespread abscessiform and necrotizing pneumonia, and bacterial (Staphylococcus aureus) endocarditis of the pulmonic valve. The right internal carotid artery was occluded by a thrombus and there were areas of necrosis due to CVAs (strokes) in the brain. | |
| − | |||
| − | Autopsy revealed severe emphysema, severe widespread abscessiform and necrotizing pneumonia, and bacterial (Staphylococcus aureus) endocarditis of the pulmonic valve. The right internal carotid artery was occluded by a thrombus and there were areas of necrosis | ||
== Images == | == Images == | ||
| Line 18: | Line 16: | ||
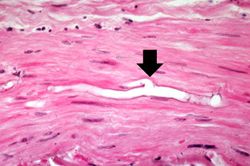
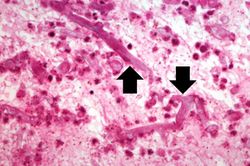
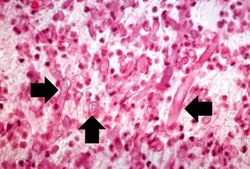
File:IPLab10Mucor8.jpg|This is another high-power photomicrograph of the thrombus stained to outline the Mucor organisms (arrows). | File:IPLab10Mucor8.jpg|This is another high-power photomicrograph of the thrombus stained to outline the Mucor organisms (arrows). | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Virtual Microscopy == | ||
| + | <peir-vm>IPLab10Mucor</peir-vm> | ||
== Study Questions == | == Study Questions == | ||
| Line 25: | Line 26: | ||
The three primary sites of Mucor invasion are the nasal sinuses, lungs, and gastrointestinal tract.</spoiler> | The three primary sites of Mucor invasion are the nasal sinuses, lungs, and gastrointestinal tract.</spoiler> | ||
* <spoiler text="What special risks of Mucor infection are associated with diabetes?">In diabetics, the fungus may spread from nasal sinuses to the orbit, and subsequently the brain, giving rise to rhinocerebral mucormycosis.</spoiler> | * <spoiler text="What special risks of Mucor infection are associated with diabetes?">In diabetics, the fungus may spread from nasal sinuses to the orbit, and subsequently the brain, giving rise to rhinocerebral mucormycosis.</spoiler> | ||
| + | |||
| + | == Additional Resources == | ||
| + | === Reference === | ||
| + | * [http://emedicine.medscape.com/article/222551-overview eMedicine Medical Library: Mucormycosis] | ||
| + | * [http://www.merckmanuals.com/professional/infectious_diseases/fungi/mucormycosis.html Merck Manual: Mucormycosis] | ||
| + | |||
| + | === Journal Articles === | ||
| + | * Marcó del Pont J, De Cicco L, Gallo G, Llera J, De Santibanez E, D'agostino D. [http://www.ncbi.nlm.nih.gov/pubmed/11429008 Hepatic arterial thrombosis due to Mucor species in a child following orthotopic liver transplantation]. ''Transpl Infect Dis'' 2000 Mar;2(1):33-5. | ||
| + | |||
| + | === Images === | ||
| + | * [{{SERVER}}/library/index.php?/tags/2158-mucormycosis PEIR Digital Library: Mucormycosis Images] | ||
| + | * [http://library.med.utah.edu/WebPath/INFEHTML/INFECIDX.html WebPath: Infection] | ||
| + | |||
| + | == Related IPLab Cases == | ||
| + | |||
{{IPLab 10}} | {{IPLab 10}} | ||
[[Category: IPLab:Lab 10]] | [[Category: IPLab:Lab 10]] | ||
Latest revision as of 21:59, 9 July 2020
Contents
Clinical Summary[edit]
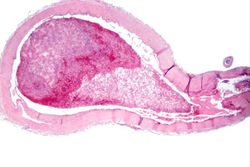
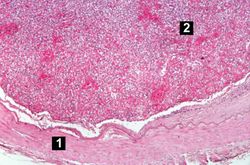
This 63-year-old white male was in his usual state of good health until eight weeks before his death when he developed sudden onset of shortness of breath. A thoracotomy was performed for plication of ruptured emphysematous blebs. Following improvement and discharge from the hospital he developed weakness, lethargy, and a left lower lobe lung infiltrate. The patient's condition soon deteriorated further, with almost every organ system having failed. The patient developed DIC and peripheral embolic phenomena, including gangrene of his extremities and face. A single antemortem blood culture grew Staphylococcus aureus.
Autopsy revealed severe emphysema, severe widespread abscessiform and necrotizing pneumonia, and bacterial (Staphylococcus aureus) endocarditis of the pulmonic valve. The right internal carotid artery was occluded by a thrombus and there were areas of necrosis due to CVAs (strokes) in the brain.
Images[edit]
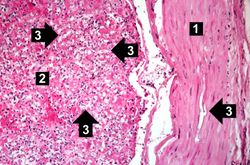
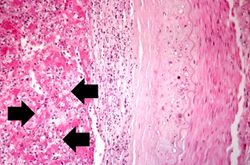
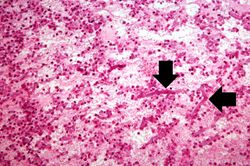
This is an even higher-power photomicrograph of the wall of the carotid artery (1) and the thrombus (2). Within the wall of the artery and in the thrombus there are multiple variably shaped clear areas (3). At this magnification and with this stain, it is impossible to determine what these clear spaces represent.
Virtual Microscopy[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
Journal Articles[edit]
- Marcó del Pont J, De Cicco L, Gallo G, Llera J, De Santibanez E, D'agostino D. Hepatic arterial thrombosis due to Mucor species in a child following orthotopic liver transplantation. Transpl Infect Dis 2000 Mar;2(1):33-5.
Images[edit]
Related IPLab Cases[edit]
| |||||
Shortness of breath is a common clinical manifestation of heart failure.
A thoracotomy is a surgical procedure in which an opening is made in the chest wall.
An infiltrate is an accumulation of cells in the lung parenchyma--this is a sign of pneumonia.
Pulmonary emphysema is a condition in which the air spaces distal to the terminal bronchioles are permanently increased in size due to either destruction of the wall or alveolar dilatation.
In alcoholics, aspiration pneumonia is common--bacteria enter the lung via aspiration of gastric contents.
A thrombus is a solid mass resulting from the aggregation of blood constituents within the vascular system.
Mural thrombosis is the formation of multiple thrombi along an injured endocardial wall.