|
|
| Line 1: |
Line 1: |
| | == Clinical Summary == | | == Clinical Summary == |
| − | The patient is an 80 year old male who presented to the Emergency Department with a chief complaint of right flank pain. He described the pain as a 10/10 pain in his right flank. He denied any associated symptoms with this pain. He denied constipation, cough, shortness of breath, fever, dysuria, hematuria, nausea, or diarrhea. He could not identify anything that made the pain worse or better. He did take 5mg of acetaminophen-hydrocodone and did not have any relief. He had just taken his evening medications when the pain began, and he can not identify any activity that may have caused the pain. | + | The patient is an 60 year old male with a remote history of an abdominal melanoma that was excised with negative margins. The patient has been experiencing lower back pain for the past several months and has received epidural injections. As a part of the workup, the patient had a CT which revealed retroperitoneal lymphadenopathy. A CT guided fine needle aspiration and biopsy of a paracaval lymph node was performed. |
| | | | |
| | === Past Medical History === | | === Past Medical History === |
| − | * Chronic obstructive pulmonary disease | + | * 2003 Melanoma |
| − | * Allergic rhinitis | + | * Diabetes |
| | * Hypertension | | * Hypertension |
| − | * Hyperlipidemia
| |
| − | * Diverticulosis
| |
| − | * Coronary artery disease
| |
| − | * Diabetes mellitus type 2
| |
| | | | |
| | === Past Surgical History === | | === Past Surgical History === |
| − | * 1993 Disk arthroplasty | + | * 2013 Arthroscopic knee surgery |
| − | * 2002 Coronary artery bypass with grafting | + | * 2003 Excision of melanoma |
| − | * 2009 arthroplasty | + | * 2002 Discectomy |
| − | * Cholecystectomy year unknown
| |
| | | | |
| − | === Medications ===
| |
| − | * Acetominophen-hydrocodone
| |
| − | * Acetaminophen-oxycodone
| |
| − | * Albuterol
| |
| − | * Aspirin
| |
| − | * Gabapentin
| |
| − | * Losartan
| |
| − | * Meloxicam
| |
| − | * Metoprolol
| |
| − | * Nitroglycerin
| |
| | | | |
| | ===Clinical Plan=== | | ===Clinical Plan=== |
| − | Differential diagnosis for flank pain includes: kidney stone, vertebral compression fracture,and infection. The suspicion for kidney stone was highest on the list. A urine culture, abdominal CT, and POC urine were ordered.
| + | The differential diagnosis for otherwise asymptomatic lymphadenopathy in this patient is melanoma, lymphoma, or occult malignancy. |
| | | | |
| | ==Radiology== | | ==Radiology== |
| − | CT scan revealed multiple lytic and sclerotic lesions within the thoracolumbar spine and sacrum. These were thought to be suspicious of metastatic disease. Wall thickening in the descending colon was seen and was thought to possibly represent a primary colon cancer. The prostate was enlarged. | + | * PET CT showed hypermetabolic activity with an SUV of 12.7. |
| − | | + | * CT of abdomen and pelvis showed adenopathy adjacent to the aorta and inferior to the vena cava at the level of the right kidney. The largest node measured 4 cm in greatest dimension. |
| − | The clinicians decided to perform a CT guided biopsy and a touch prep was made for rapid interpretation by the Cytology team.
| |
| | | | |
| | ===CT=== | | ===CT=== |
| Line 54: |
Line 38: |
| | | | |
| | ====Resident Questions==== | | ====Resident Questions==== |
| − | * <spoiler text="Benign or malignant?">These groups of cohesive cells are larger than the normal elements we would expect to find in a touch prep from a spinal biopsy. This, along with the patient's history, should make you think that there is a malignant process involving the spine.</spoiler> | + | * <spoiler text="What is your differential diagnosis?">These groups of cells demonstrate malignant appearing cells in a background of an otherwise benign appearing lymphoid background. The atypical cells are scattered, with large nucleoli and several binucleate forms. In addition, there seem to be an increased number of eosinophils in the background. The differential diagnosis includes Hodgkin lymphoma; however, the possibility of the large atypical cells being melanoma cannot be ruled out. </spoiler> |
| | * <spoiler text="What would you call this on a Rapid Interpretation?">This is a male patient with no previous history of malignancy. Our differential diagnosis can include many entities. However, these are cohesive cells so lymphoma should be at the bottom of our list. We would need more information to classify these cells, but a diagnosis of positive for malignancy (with no further specificity) can be rendered.</spoiler> | | * <spoiler text="What would you call this on a Rapid Interpretation?">This is a male patient with no previous history of malignancy. Our differential diagnosis can include many entities. However, these are cohesive cells so lymphoma should be at the bottom of our list. We would need more information to classify these cells, but a diagnosis of positive for malignancy (with no further specificity) can be rendered.</spoiler> |
| | | | |
Clinical Summary
The patient is an 60 year old male with a remote history of an abdominal melanoma that was excised with negative margins. The patient has been experiencing lower back pain for the past several months and has received epidural injections. As a part of the workup, the patient had a CT which revealed retroperitoneal lymphadenopathy. A CT guided fine needle aspiration and biopsy of a paracaval lymph node was performed.
Past Medical History
- 2003 Melanoma
- Diabetes
- Hypertension
Past Surgical History
- 2013 Arthroscopic knee surgery
- 2003 Excision of melanoma
- 2002 Discectomy
Clinical Plan
The differential diagnosis for otherwise asymptomatic lymphadenopathy in this patient is melanoma, lymphoma, or occult malignancy.
Radiology
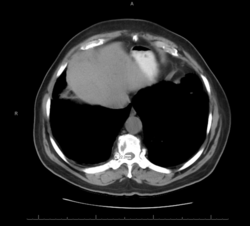
- PET CT showed hypermetabolic activity with an SUV of 12.7.
- CT of abdomen and pelvis showed adenopathy adjacent to the aorta and inferior to the vena cava at the level of the right kidney. The largest node measured 4 cm in greatest dimension.
CT
Pathology
Cytology
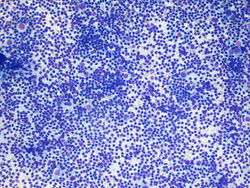
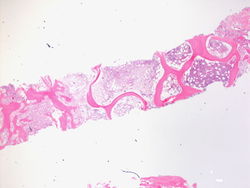
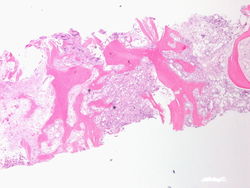
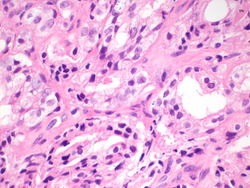
10x magnification of paracaval lymph node. There is a polymorphic lymphoid population with scattered large atypical cells.
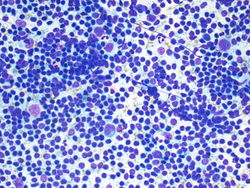
20x magnification of paracaval lymph node. There are small lymphocytes with background lymphoglandular bodies. Scattered eosinophils and large atypical cells with prominent nucleoli.
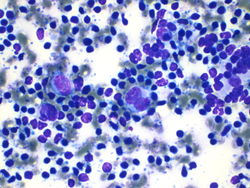
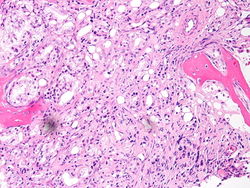
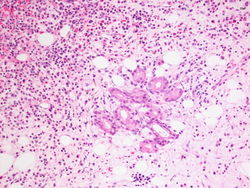
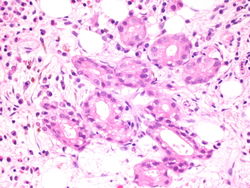
40x magnification of paracaval lymph node. There are atypical binucleated cells among the large atypical cells.
Resident Questions
These groups of cells demonstrate malignant appearing cells in a background of an otherwise benign appearing lymphoid background. The atypical cells are scattered, with large nucleoli and several binucleate forms. In addition, there seem to be an increased number of eosinophils in the background. The differential diagnosis includes Hodgkin lymphoma; however, the possibility of the large atypical cells being melanoma cannot be ruled out.
This is a male patient with no previous history of malignancy. Our differential diagnosis can include many entities. However, these are cohesive cells so lymphoma should be at the bottom of our list. We would need more information to classify these cells, but a diagnosis of positive for malignancy (with no further specificity) can be rendered.
Biopsy
This is a 2x magnification the biopsy specimen from the spinal mass. We see that this is bone histology which is abnormal. There is an increase in cellularity, especially for an 80 year old person.
This is a 4x magnification of the biopsy specimen from the spinal mass. We can see that there is an increase in cellularity.
This is a 20x magnification of the biopsy specimen from the spinal mass. This is one of the areas that has increased cellularity on lower power. We can see cells forming what appear to be glands in the bone marrow.
This is a 20x magnification of the biopsy specimen from the spinal mass. Here we see well formed glands in the bone marrow.
This is a 60x magnification of the biopsy specimen from the spinal mass. The malignant cells appear to be creating glandular structures, and we can identify prominent nucleoli in the malignant cells.
This is a 60x magnification of the biopsy specimen from the spinal mass. Again we see well formed glands in the bone marrow, made of cells that have prominent nucleoli.
Immunohistochemistry
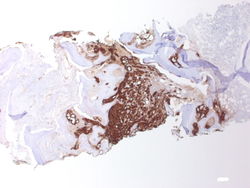
PSA, 2x magnification. Note the predominance of brown staining in the middle.
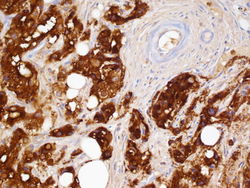
PSA, 60x magnification. The glands are highlighted in brown, and on the upper right the blood vessels are negative.
Resident Questions
This is a male patient with a new spinal mass. The spinal mass has glands made of cells with prominent nucleoli. In a case like this you should consider prostate as the source of the malignancy. A PSA stain would help highlight cells of prostatic origin.
Click here to toggle the diagnosis and case discussion.
Final Diagnosis
Cytology
Biopsy
- Metastatic prostatic adenocarcinoma.
Case Discussion
This is a classic case of prostatic adenocarcinoma, metastatic to the spine.