Difference between revisions of "IPLab:Lab 10:Candidiasis"
(→Clinical Summary) |
|||
| (10 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
== Clinical Summary == | == Clinical Summary == | ||
| + | This 73-year-old black male was in good health until about three months before his death when he noticed enlarged lymph nodes first in both inguinal regions and later elsewhere. Antileukemic therapy was begun. About two weeks prior to his death the patient presented to the emergency room with uncontrollable epistaxis. On physical examination, the liver was palpable but the spleen was not. The white blood count was below normal and consisted mainly of lymphocytes with many atypical cells. The patient's bone marrow was also found to be heavily loaded with lymphocytes. Platelets were extremely low and remained so despite platelet transfusions. Subsequently, the patient developed pneumonia which progressed until death. Antemortem cultures yielded Candida tropicalis and Pseudomonas aeruginosa. | ||
| − | + | At autopsy, there was evidence of disseminated candidiasis. | |
| − | |||
| − | |||
| − | |||
| − | At autopsy, there was evidence of disseminated candidiasis. | ||
== Images == | == Images == | ||
| Line 18: | Line 15: | ||
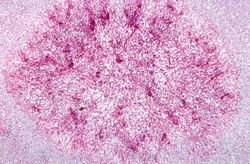
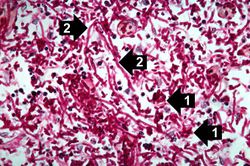
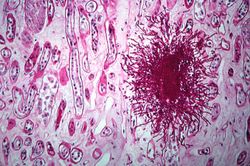
File:IPLab10Candidiasis8.jpg|This is a higher-power photomicrograph of a Candida colony in the kidney. Note the pseudohyphae of the Candida organisms. | File:IPLab10Candidiasis8.jpg|This is a higher-power photomicrograph of a Candida colony in the kidney. Note the pseudohyphae of the Candida organisms. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Virtual Microscopy == | ||
| + | <peir-vm>IPLab10Candidiasis</peir-vm> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="What is the significance of seeing yeast and hyphae in these histologic tissue sections?">Candida is the only fungus which grows as: | ||
| + | # a yeast form, | ||
| + | # pseudohyphae, and | ||
| + | # true hyphae with septa. | ||
| + | |||
| + | All three of these forms may be present in the same section of tissue.</spoiler> | ||
| + | * <spoiler text="Who is at risk for developing systemic candidiasis?">Neutropenic patients. | ||
| + | |||
| + | Candida species--especially C. albicans--are part of the normal flora of the skin, mouth, and GI tract, and are the most frequent cause of human fungal infections. These infections vary from superficial lesions in healthy persons to disseminated infections in neutropenic patients. | ||
| + | |||
| + | Severe disseminated candidiasis is associated with neutropenia secondary to chronic granulomatous disease, leukemia, anticancer therapy, or immunosuppression after transplantation. | ||
| + | |||
| + | Candida can be introduced into the bloodstream by intravenous lines, catheters, peritoneal dialysis, cardiac surgery, or intravenous drug abuse.</spoiler> | ||
| + | * <spoiler text="What types of infections does Candida cause in humans?">Candida infections can occur in the oral cavity (thrush), vagina, and in the skin--especially in warm moist areas (i.e., between the fingers and toes and in inguinal creases, inframammary folds, and the anogenital region). | ||
| + | |||
| + | Candida esophagitis can occur with nasogastric tube placement.</spoiler> | ||
| + | |||
| + | == Additional Resources == | ||
| + | === Reference === | ||
| + | * [http://emedicine.medscape.com/article/781215-overview eMedicine Medical Library: Candidiasis in Emergency Medicine] | ||
| + | * [http://emedicine.medscape.com/article/213853-overview eMedicine Medical Library: Candidiasis] | ||
| + | * [http://www.merckmanuals.com/professional/infectious_diseases/fungi/candidiasis_invasive.html Merck Manual: Candidiasis (Invasive)] | ||
| + | |||
| + | === Journal Articles === | ||
| + | * Marr KA, Bowden RA. [http://www.ncbi.nlm.nih.gov/pubmed/11428995 Fungal infections in patients undergoing blood and marrow transplantation]. ''Transpl Infect Dis'' 1999 Dec;1(4):237-46. | ||
| + | * Marr KA, Bowden RA. [http://www.nejm.org/doi/full/10.1056/NEJMra1315399 Invasive Candidiasis]. ''NEJM'' 2015 Oct 8;373:1445-1456. | ||
| + | |||
| + | === Images === | ||
| + | * [{{SERVER}}/library/index.php?/tags/2156-candidiasis PEIR Digital Library: Candidiasis] | ||
| + | * [http://library.med.utah.edu/WebPath/INFEHTML/INFECIDX.html Webpath: Infection] | ||
{{IPLab 10}} | {{IPLab 10}} | ||
[[Category: IPLab:Lab 10]] | [[Category: IPLab:Lab 10]] | ||
Latest revision as of 21:45, 9 July 2020
Contents
Clinical Summary[edit]
This 73-year-old black male was in good health until about three months before his death when he noticed enlarged lymph nodes first in both inguinal regions and later elsewhere. Antileukemic therapy was begun. About two weeks prior to his death the patient presented to the emergency room with uncontrollable epistaxis. On physical examination, the liver was palpable but the spleen was not. The white blood count was below normal and consisted mainly of lymphocytes with many atypical cells. The patient's bone marrow was also found to be heavily loaded with lymphocytes. Platelets were extremely low and remained so despite platelet transfusions. Subsequently, the patient developed pneumonia which progressed until death. Antemortem cultures yielded Candida tropicalis and Pseudomonas aeruginosa.
At autopsy, there was evidence of disseminated candidiasis.
Images[edit]
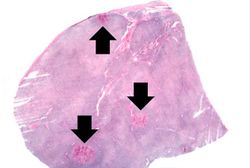
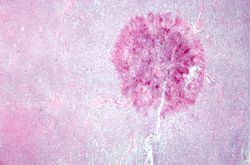
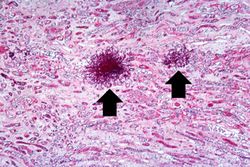
This is a low-power photomicrograph of lymph node with three prominent areas of Candida colonies (arrows). Even at this low magnification, the purple-staining yeast and pseudohyphae can be easily seen. This section was stained with Periodic Acid-Schiff Hematoxylin (PASH ), which stains the cell wall of fungi to make them more easily visible.
Virtual Microscopy[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Candidiasis in Emergency Medicine
- eMedicine Medical Library: Candidiasis
- Merck Manual: Candidiasis (Invasive)
Journal Articles[edit]
- Marr KA, Bowden RA. Fungal infections in patients undergoing blood and marrow transplantation. Transpl Infect Dis 1999 Dec;1(4):237-46.
- Marr KA, Bowden RA. Invasive Candidiasis. NEJM 2015 Oct 8;373:1445-1456.
Images[edit]
| |||||
Epistaxis is bleeding from the nose.
In alcoholics, aspiration pneumonia is common--bacteria enter the lung via aspiration of gastric contents.