Difference between revisions of "IPLab:Lab 11:Malaria"
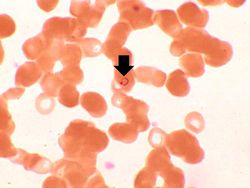
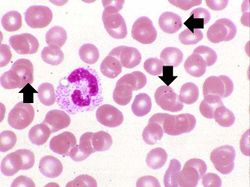
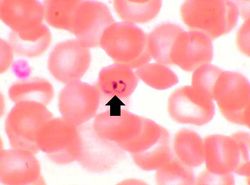
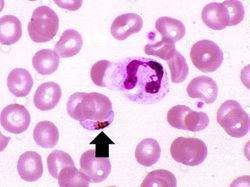
Seung Park (talk | contribs) (Created page with "== Images == <gallery heights="250px" widths="250px"> File:IPLab11Malaria1.jpg|This is a high power photomicrograph of a thin smear of blood from this patient. Note that one o...") |
Seung Park (talk | contribs) |
||
| (9 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
| + | == Clinical Summary == | ||
| + | This 46-year-old forestry consultant presented with a seven-day history of mild abdominal cramping, diarrhea, mild myalgias, gradually worsening headache, and subjective fever. The patient had recently returned from spending 5 months in the Thailand rainforests as a consultant to lumber companies. Stool cultures and repeated stool examinations for ova and parasites were negative. A presumptive diagnosis of viral gastroenteritis was made. Three days later the patient returned with a fever of 103° and bloody diarrhea. On examination the patient appeared acutely ill and had orthostatic hypotension. Exam was otherwise unremarkable. The patient was admitted and intravenous rehydration and broad-spectrum IV antibiotics were begun. Over the next eight hours the patient became progressively lethargic and finally became unresponsive to speech. His temperature rose to 106°. Careful examination of a peripheral blood smear revealed P. falciparum with a parasitemia of 5%. Intravenous antimalarial drugs were administered and over the next three days the patient's clinical condition gradually improved. Repeat peripheral smears at 3, 7, 14, and 28 days were negative for malaria. | ||
| + | |||
== Images == | == Images == | ||
<gallery heights="250px" widths="250px"> | <gallery heights="250px" widths="250px"> | ||
| Line 9: | Line 12: | ||
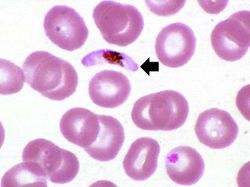
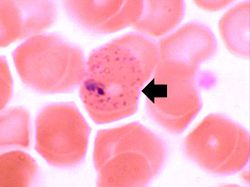
File:IPLab11Malaria7.jpg|In this peripheral smear from a different patient who was infected with P. vivax, the cytoplasm of the infected RBC has a stippled appearance (Schüffner's dots) (arrow). The RBC is also slightly enlarged. | File:IPLab11Malaria7.jpg|In this peripheral smear from a different patient who was infected with P. vivax, the cytoplasm of the infected RBC has a stippled appearance (Schüffner's dots) (arrow). The RBC is also slightly enlarged. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Virtual Microscopy == | ||
| + | <peir-vm>IPLab11Malaria</peir-vm> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="This man had been taking appropriate malaria chemoprophylaxis during his stay in Thailand. Why did the patient get malaria nonetheless?">He could have gotten malaria because some malaria organisms have developed resistance to commonly used antimalarial drugs. Another common cause is noncompliance -- travelers forget to take their drugs!</spoiler> | ||
| + | * <spoiler text="What was the possible mechanism for the dysentery that developed in this patient?">Parasitized red blood cells cause obstruction of small blood vessels in the bowel leading to bowel ischemia. Another possible cause for dysentery in someone just back from a third world country would be intestinal parasites, such as Giardia, Entamoeba, or helminths.</spoiler> | ||
| + | * <spoiler text="What was the probable cause of the patient's altered mental status?">Patients with very high fever can develop altered metal status, but in this case the likely cause would be malignant cerebral malaria. Parasitized RBCs block small blood vessels in the brain leading to multifocal areas of hypoxia.</spoiler> | ||
| + | |||
| + | == Additional Resources == | ||
| + | === Reference === | ||
| + | * [http://emedicine.medscape.com/article/221134-overview eMedicine Medical Library: Malaria] | ||
| + | * [http://emedicine.medscape.com/article/784065-overview eMedicine Medical Library: Emergent Management of Malaria] | ||
| + | * [http://www.merckmanuals.com/professional/infectious_diseases/extraintestinal_protozoa/malaria.html Merck Manual: Malaria] | ||
| + | * [http://www.cdc.gov/parasites/ Centers for Disease Control and Prevention: Parasites] | ||
| + | |||
| + | === Journal Articles === | ||
| + | * Mishra SK, Mohanty S, Mohanty A, Das BS. [http://www.ncbi.nlm.nih.gov/pubmed/17102547 Management of severe and complicated malaria]. ''J Postgrad Med'' 2006 Oct-Dec;52(4):281-7. | ||
| + | |||
| + | === Images === | ||
| + | * [{{SERVER}}/library/index.php?/tags/2159-malaria PEIR Digital Library: Malaria Images] | ||
| + | * [http://library.med.utah.edu/WebPath/INFEHTML/INFECIDX.html Webpath: Infection] | ||
{{IPLab 11}} | {{IPLab 11}} | ||
[[Category: IPLab:Lab 11]] | [[Category: IPLab:Lab 11]] | ||
Latest revision as of 16:36, 3 January 2014
Contents
Clinical Summary
This 46-year-old forestry consultant presented with a seven-day history of mild abdominal cramping, diarrhea, mild myalgias, gradually worsening headache, and subjective fever. The patient had recently returned from spending 5 months in the Thailand rainforests as a consultant to lumber companies. Stool cultures and repeated stool examinations for ova and parasites were negative. A presumptive diagnosis of viral gastroenteritis was made. Three days later the patient returned with a fever of 103° and bloody diarrhea. On examination the patient appeared acutely ill and had orthostatic hypotension. Exam was otherwise unremarkable. The patient was admitted and intravenous rehydration and broad-spectrum IV antibiotics were begun. Over the next eight hours the patient became progressively lethargic and finally became unresponsive to speech. His temperature rose to 106°. Careful examination of a peripheral blood smear revealed P. falciparum with a parasitemia of 5%. Intravenous antimalarial drugs were administered and over the next three days the patient's clinical condition gradually improved. Repeat peripheral smears at 3, 7, 14, and 28 days were negative for malaria.
Images
Virtual Microscopy
Study Questions
Additional Resources
Reference
- eMedicine Medical Library: Malaria
- eMedicine Medical Library: Emergent Management of Malaria
- Merck Manual: Malaria
- Centers for Disease Control and Prevention: Parasites
Journal Articles
- Mishra SK, Mohanty S, Mohanty A, Das BS. Management of severe and complicated malaria. J Postgrad Med 2006 Oct-Dec;52(4):281-7.
Images
| |||||