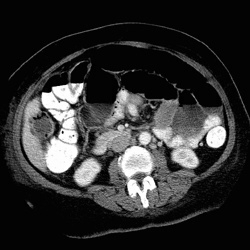
RADIOLOGY: HEPATOBILIARY: Case# 54: GANGRENOUS/EMPHYSEMATOUS CHOLECYSTITIS & PELVIC MASS. 66 year old female with a history of squamous cell carcinoma of the cervix who presents with fever and abdominal pain. The gallbladder has irregular wall thickening and contains bubbles of air. Pericholecystic fluid is seen adjacent to the lateral abdominal wall. These findings are consistent with gangrenous cholecystitis with perforation. Acute cholecystitis, or inflammation of the gallbladder, can be classified as calculous (associated with gallstones) or acalculous. Gangrenous cholecystitis is a rare form of acute cholecystitis which is often indistinguishable from acute cholecystitis. The mortality rate of gangrenous cholecystitis is 22% while the mortality rate for acute cholecystitis is only around 1 to 6%. Symptoms associated with the onset of acute cholecystitis include progressive right upper quadrant or epigastric pain, mild fever, anorexia, tachycardia, diaphoresis, and nausea and vomiting. Lab abnormalities associated with this condition include mild to moderate leukocytosis often accompanied by mild elevations in serum alkaline phosphatase values. Most cases of acute cholecystitis are diagnosed clinically, via ultrasound, or via radionuclide hepatobiliary scan. CT is used to evaluate complicated or atypical cases. CT findings include gallstones (in 95% of patients), distended gallbladder lumen (greater than 5cm), thickening of the gallbladder wall (greater than 3mm), halo of subserosal edema in the gallbladder wall, pericholecystic fluid collection associated with perforation, increase in bile density to ~20 HU (due to biliary stasis, intraluminal pus, hemorrhage or cellular debris), and air in the gallbladder wall (emphysematous cholcystitis).
- Author
- Peter Anderson
- Posted on
- Thursday 1 August 2013
- Tags
- hepatobiliary, radiology
- Albums
- Visits
- 1323


0 comments