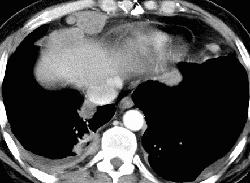
RADIOLOGY: CHEST: Case# 11: MALIGNANT THYMOMA W/ LUNG METS. 59 year old male with right lateral flank and chest pain. There is a right postero-basilar pleural nodularity and thickening consistent with extensive metastatic spread. A small pleural effusion is present between the thickened visceral and parietal pleurae. Several parenchymal pulmonary nodules are present within the right base in addition to the pleural nodularity. A paravertebral metastasis on the right enters the spinal canal at approximately the T11-12 level (not shown) Numerous foci of low attenuation throughout the liver measuring less than 1 cm. Thymoma is a common anterior mediastinal mass occurring primarily in adults. They may also occur in the middle or posterior mediastinum. It is often difficult to determine if a thymoma is benign or malignant based on histologic findings. Signs of local invasion are more accurate in determining malignancy, a state which is usually established at surgery. Recurrence to pleura and or mediastinum is the rule with invasive tumors. There is a strong association between thymoma and myasthenia gravis. Other associated syndromes are red cell hypoplasia and hypogammaglobulinemia. Thymoma is usually visible in the prevascular space and also in the precardiac location and is visualized as a unilateral, localized bulge containing calcifications and cystic degeneration. Bilateral, poorly defined, large lobulated masses suggest malignancy. CT may detect tumors that are invisible on plain radiograph in patients with myasthenia gravis. Small thymomas may be difficult to distinguish from normal or hyperplastic glands. In addition, they appear similar to thymic carcinoid tumors and thymolipomas. Thymolipomas are readily distinguished, however, by their fat content. Thymic cysts generally show water density on CT, but may also show soft tissue density, giving the appearance of a thymoma which may show water or soft tissue density. Cysts, however, usually have thin walled whereas thymomas will have thick or irregular walls
- Author
- Peter Anderson
- Posted on
- Thursday 1 August 2013
- Albums
- Visits
- 3991

0 comments