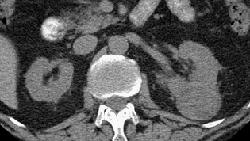
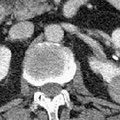
RADIOLOGY: KIDNEY: Case# 32919: RCC. This is a 66 year old male with a known renal cell carcinoma in his left kidney. On previous CT reports he also has nodules in his lung. Patient is on oral chemotherapy regiment and this is a follow-up study. Comparison is made with a prior CT. There is a 3.5 x 4.5cm mass arising from the mid left kidney. This mass is unchanged in size and appearance since the prior study. There is a simple cyst in the right kidney arising from the lower pole. There is also a simple cyst in the left kidney arising just above the pelvis. 85% of renal neoplasms are renal cell carcinomas, most commonly occurring in men, at ages 50-70, and usually involving one kidney. Only 2% are bilateral. Metastases are present at the time of diagnosis in 40% of cases. Since surgery is the only cure, early detection and accurate staging are important. The most common CT finding is a solid mass although low density areas due to hemorrhage or necrosis may be present. Cystic and multicystic forms may be seen. Stippled central or "eggshell" peripheral calcifications are seen in 10%. These tumors are usually hypervascular which may be evidenced by the presence of tortuous vessels in the perirenal fat. Tumor growth into the renal vein occurs in 30% of the time and into the inferior vena cava 5-10%. Venous invasion does not preclude surgical resection, but its identification is crucial to surgical planning. Renal cell carcinomas may spread locally to perirenal fat and adjacent organs. This is seen as strand or nodules of low density. Enlargement of renal hilar, pericaval, and periaortic nodes to 15mm or more indicates lymphatic spread. Hematogenous spread to the lung, bone, liver, adrenals, and the opposite kidney may occur. Distant metastases occasionally disappear with the removal of the primary tumor. Late appearance of metastases as long as 20 years following "cure" is also seen.
- Author
- Peter Anderson
- Posted on
- Thursday 1 August 2013
- Tags
- adrenal hemorrhage, kidney, radiology
- Albums
- Visits
- 3231

0 comments